PVC / VT ablation
PVC ablation is usually reserved for people with >10% PVC burden with adequate symptoms. Ablation can also be considered for ventricular tachycardia especially if people have progressed through medical therapy. In general, PVC ablation is effective. Procedural success in people with structural VT can be variable with one or two procedures depending on a few factors.
Please refer to the catheter ablation section for general information about the admission process and requirements.
What are the risks of having a PVC ablation?
They include but are not limited to the following.
Common risks and complications (more than 5%) include:
- Bruising bleeding at the puncture site. Bruising can extend beyond the puncture site and can take a few weeks to improve in some cases.
Uncommon risks and complications (1- 5%) include:
- Development of another arrhythmia
- A hole is made in the heart (tamponade) or heart valve. This will need surgery to repair
- Chest pain
- Stroke
- Major bleeding related to the groin puncture site or injury to an artery in the groin. This (rarely) may need surgery and or blood transfusion
- A stroke. This may cause long term disability
- Blood clot in the leg (DVT) causing pain and swelling. In rare cases part of the clot may break off and go to the lungs called pulmonary embolus
- Skin injury from radiation. This may cause reddening of the skin
- Kidney injury that may or may not be reversible (due to contrast or emboli)
- Peripheral emboli – clot travelling to distal parts of the body affecting circulation requiring emergency surgery
Rare risks and complications (less than 1-2%) include:
- Heart attack
- Internal bleeding requiring an operation
- Injury to the food pipe related to the ultrasound or temperature probe used during the procedure
- Injury to the urinary tract if a urinary catheter is required for the procedure
- Death because of this procedure is rare
- Infection from vascular closure device (if used) leading to prolonged clinical sequelae
What happens during the procedure?
Local anaesthetic is administered at the groin which numbs the area. Three to four small tubes called sheaths are passed into the vein in the right groin through which catheters are inserted and gently passed up until they reach your heart. One larger sheath may be required from the left groin in some cases for special catheter called intra cardiac echocardiogram (ICE). In many cases we will need to place another sheath in the artery if the PVC / VT originates from the left chamber (retrograde approach). An X-ray machine guides the catheters to your heart. In some cases, a special ultrasound camera called a trans oesophageal echo (TOE) probe is advanced via your mouth into your oesophagus (gullet) that sits next to your heart. The TOE is used to guide the wires across from the right side to the left atrium (LA) through a thin membrane called the interatrial septum. A long needle maybe used to get access across the septum for an antegrade or transseptal approach.
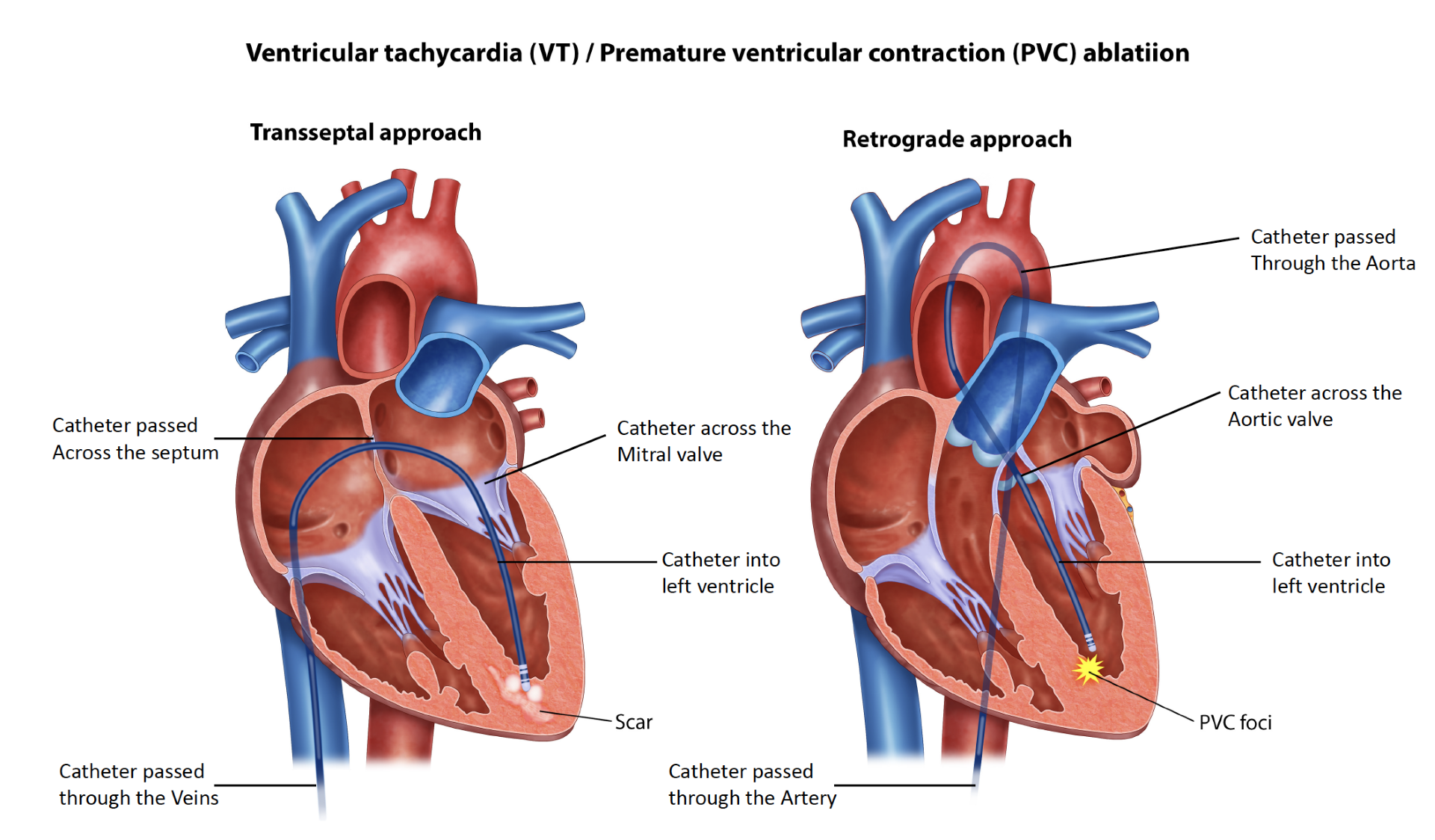
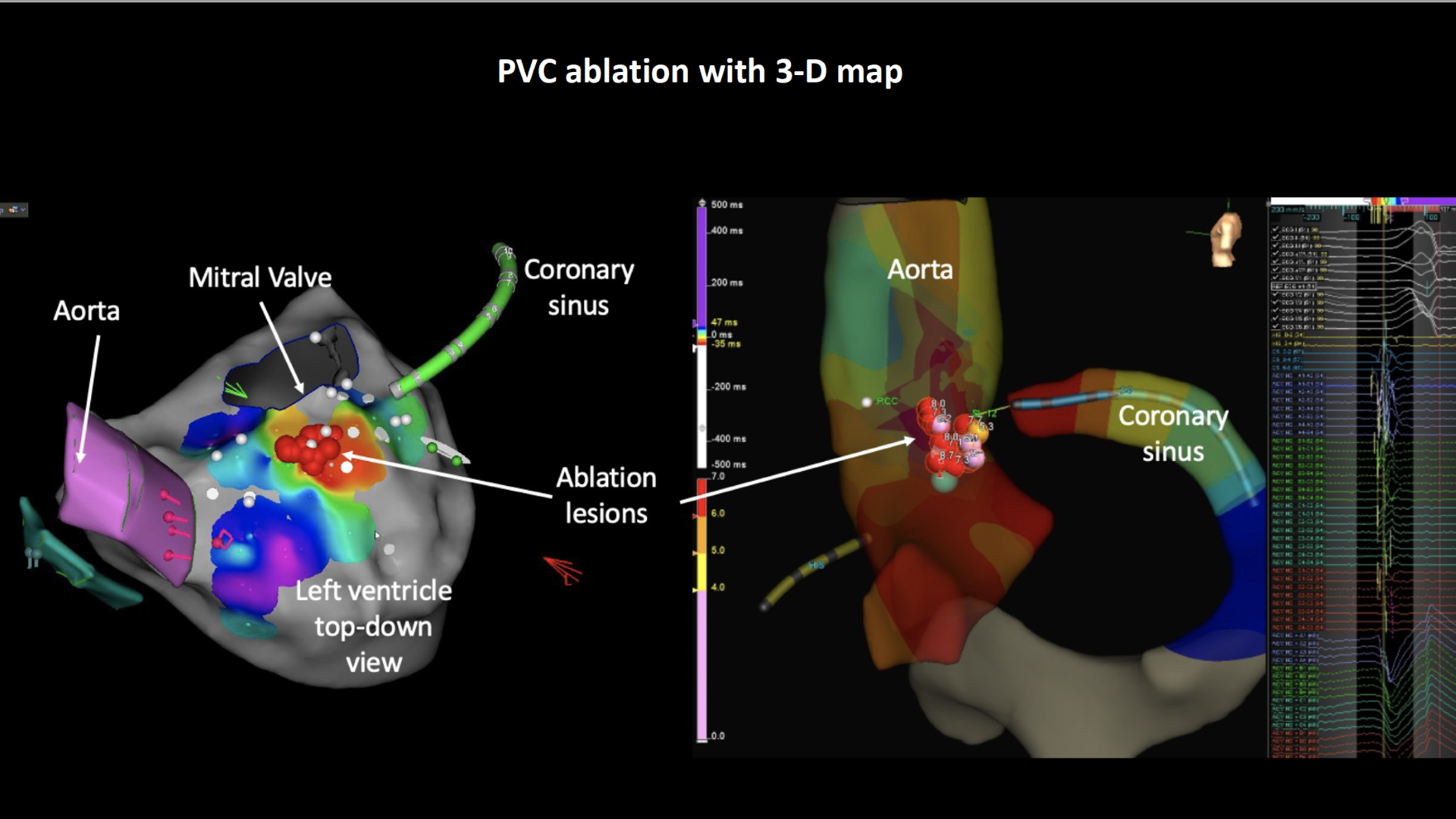
Additional blood thinners are given to thin the blood further to prevent a stroke. The TOE probe is subsequently removed. A mapping catheter is advanced into the heart to make a 3-D model which identifies the relevant structures. An ablation catheter is advanced into the heart that applies the ablation energy to the area of interest.
The catheter ablation procedure can take about 3-4hrs or more in some cases. We use contrast injection to identify he vessels and puncture level in the artery to determine a special seal can be applied to the arterial puncture site to reduce bleeding complications and to allow you to sit up sooner. This plug or stitch is called Angio-seal or Perclose. There is a small risk of infection associated with placing a plug in the artery but is rare. Extra precautions are taken at the time of deployment.
What happens after an ablation?
At the end of your procedure, your doctor will remove the catheters and apply pressure, followed by a dressing. You may have a little device applying pressure at the puncture site for a few hours. You’ll be watched closely in a recovery area, and depending on how you feel, you might need to rest in bed for a while. You will be admitted to the ward for observation overnight with rhythm monitoring. You may be required to lay flat on your back for about 4 hours after your procedure. People are usually discharged the next day.
What happens after discharge?
Follow up:
- An appointment will be made for you to be seen in clinic about 2 months after the procedure
- You will need to have follow up appointment with your usual pacemaker clinic
- If you do not receive a date for an appointment within 8 weeks, please call the clinic and ask to speak to the secretary
Medications:
- Continue your medications as instructed. If you are uncertain about your medications, please ring the rooms for clarification
Postoperative care:
- Avoid strenuous exercise for 1 week
- Start with gentle exercise after 1 weeks – e.g. walking.
Symptoms to monitor:
- It is not uncommon to have a bruise at the groin that extends / spreads after the ablation. This usually resolves over time without any other problems.
Bleeding:
- It is rare to have severe bleeding from the puncture site once you are at home. If bleeding does occur you must: lie flat, apply pressure to the site for 10 minutes. If it continues, call an ambulance for assistance.
Please contact the rooms if you have any questions or concerns at any time.
In recommending this procedure your doctor has balanced the benefits and risks of the procedure against the benefits and risks of not proceeding. Your doctor believes there is a net benefit to you going ahead. This is a very complicated assessment.