Ventricular tachycardia (VT)
What is Ventricular tachycardia (VT)?
Ventricular tachycardia (VT) is an abnormal rhythm characterized by sustained, rapid, and regular heartbeats originating from the ventricles, the lower chambers of the heart. It can occur in individuals with a structurally normal heart, where the abnormal rhythm is caused by a group of rogue active cells continuously stimulating the heart. For more information, please refer to the section on premature ventricular contractions (PVCs).
In most cases, VT is more commonly observed in individuals with a structurally abnormal or scarred heart. The heart, being a muscular organ, can sustain damage and develop areas of scar tissue. These scarred regions often exhibit irregularities and contain small pockets of living tissue that form channels. The normal electrical signals that are meant to smoothly propagate through the heart muscle can get trapped within these channels or islands, creating a looped circuit. This continuous loop of electrical signals gives rise to VT. It is possible to have multiple circuits of VT occurring simultaneously.
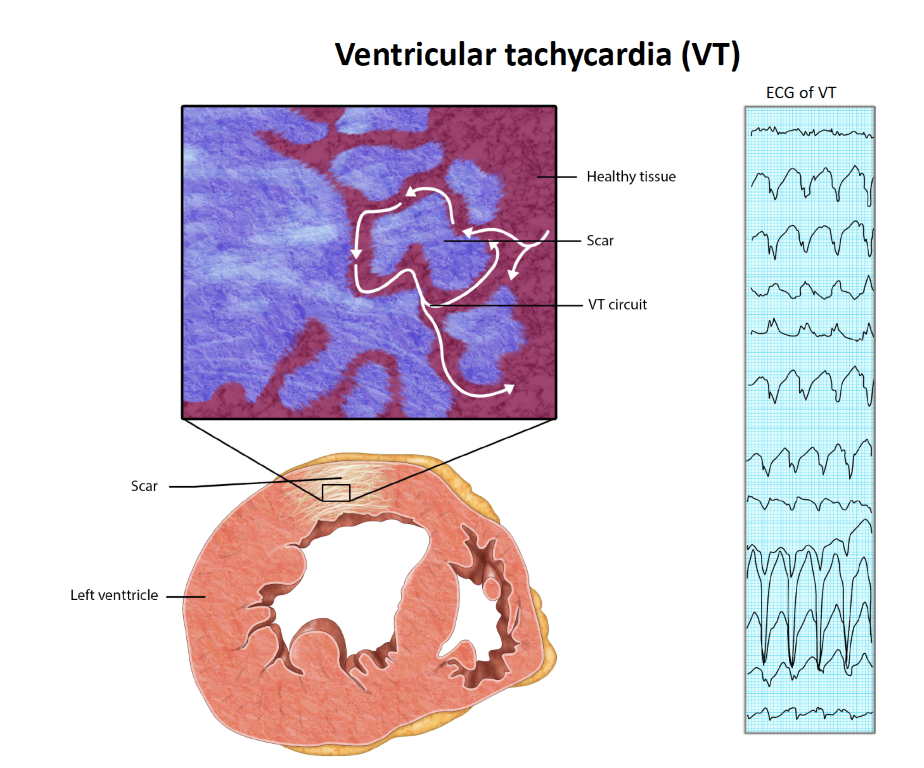
Scar tissue can result from various conditions, including heart attacks caused by blocked arteries, inflammatory conditions such as myocarditis, and certain genetic conditions like hypertrophic cardiomyopathy and non-ischemic cardiomyopathy. These factors contribute to the development of abnormal electrical pathways within the heart, leading to the occurrence of VT.
Non-sustained ventricular tachycardia (NSVT) refers to episodes of VT that last less than 30 seconds. It is not uncommon for individuals, including those who are healthy and asymptomatic, to experience NSVT. The presence of NSVT alone does not automatically indicate the need for treatment. It is important to evaluate the overall clinical context, including the individual’s medical history, symptoms, and any associated underlying conditions, to determine the appropriate course of action. Short runs of NSVT lasting less than a few seconds is a common.
What are the consequences of VT?
Ventricular tachycardia occurring in individuals with scarred or structurally abnormal hearts is a condition of significant concern. It is widely recognised as a dangerous and potentially life-threatening condition. The presence of ventricular tachycardia is often associated with symptoms such as loss of consciousness, palpitations, shortness of breath, chest pain, and heart failure. It is important to note that ventricular tachycardia has the potential to deteriorate into a more chaotic rhythm known as ventricular fibrillation (VF), which can be fatal. In the case of ventricular fibrillation, immediate defibrillation is typically required to restore a normal heart rhythm and facilitate recovery. Prompt medical attention and intervention are crucial in managing ventricular tachycardia and preventing its progression to ventricular fibrillation.
Is VT dangerous?
In people with structural heart disease, VT can be potentially dangerous. However, with medications and cardiac devices such as defibrillators, it is usually a well-managed condition.
What are the treatment options available for VT?
Medical care:
Managing individuals with VT is a complex process that typically requires the involvement of multiple healthcare professionals with specialised expertise. In cases where there is concurrent heart failure, it is common to have a team of medical practitioners collaborating on your care. This team may consist of a cardiac interventionalist, a heart failure specialist, and an electrophysiologist, each bringing their specific knowledge and skills to address the various aspects of your condition. By working together, these professionals can provide comprehensive and coordinated care tailored to your individual needs.
Cardiac devices:
A crucial aspect of managing ventricular tachycardia (VT) in individuals with a structurally abnormal heart involves considering the use of a defibrillator.

Known as an implantable cardioverter-defibrillator (ICD), a defibrillator consists of two sophisticated components: the lead and the generator, which functions as the control centre and houses the battery unit. This implantable device is capable of detecting, analysing, stimulating, and, if necessary, delivering an electrical shock to restore the heart’s normal rhythm during sustained ventricular tachycardia. Think of defibrillators as an insurance policy—they are present as a safeguard in case you have further VT despite medications and other interventions. It is important to understand that defibrillators do not prevent abnormal rhythms; rather, they remain on standby, ready to treat abnormal rhythms if medications fail to suppress them.
Medications:
People with ventricular tachycardia (VT) often require medication as part of their treatment plan. The specific medications prescribed can vary, ranging from simpler options to more advanced and targeted therapies such as amiodarone and other medications that specifically address abnormal heart rhythms. Additionally, optimising the treatment of any underlying heart condition can contribute to better management of VT. It is important to work closely with your healthcare provider to determine the most appropriate medication regimen and overall treatment approach based on your individual circumstances and medical needs.
Procedural options:
Catheter ablation is a frequently performed minimally invasive procedure that aims to identify and ablate the abnormal foci responsible for VT in order to prevent its recurrence. The effectiveness of the procedure can vary depending on the specific location, but typically ranges from 60% to 80% with one or two procedures. In certain cases, more advanced forms of ablation, such as epicardial ablation, may be necessary. However, it is important to note that epicardial ablation is only performed at selected sites and is not the standard approach for all cases.