What is an implantable cardioverter-defibrillator (ICD) / defibrillator?
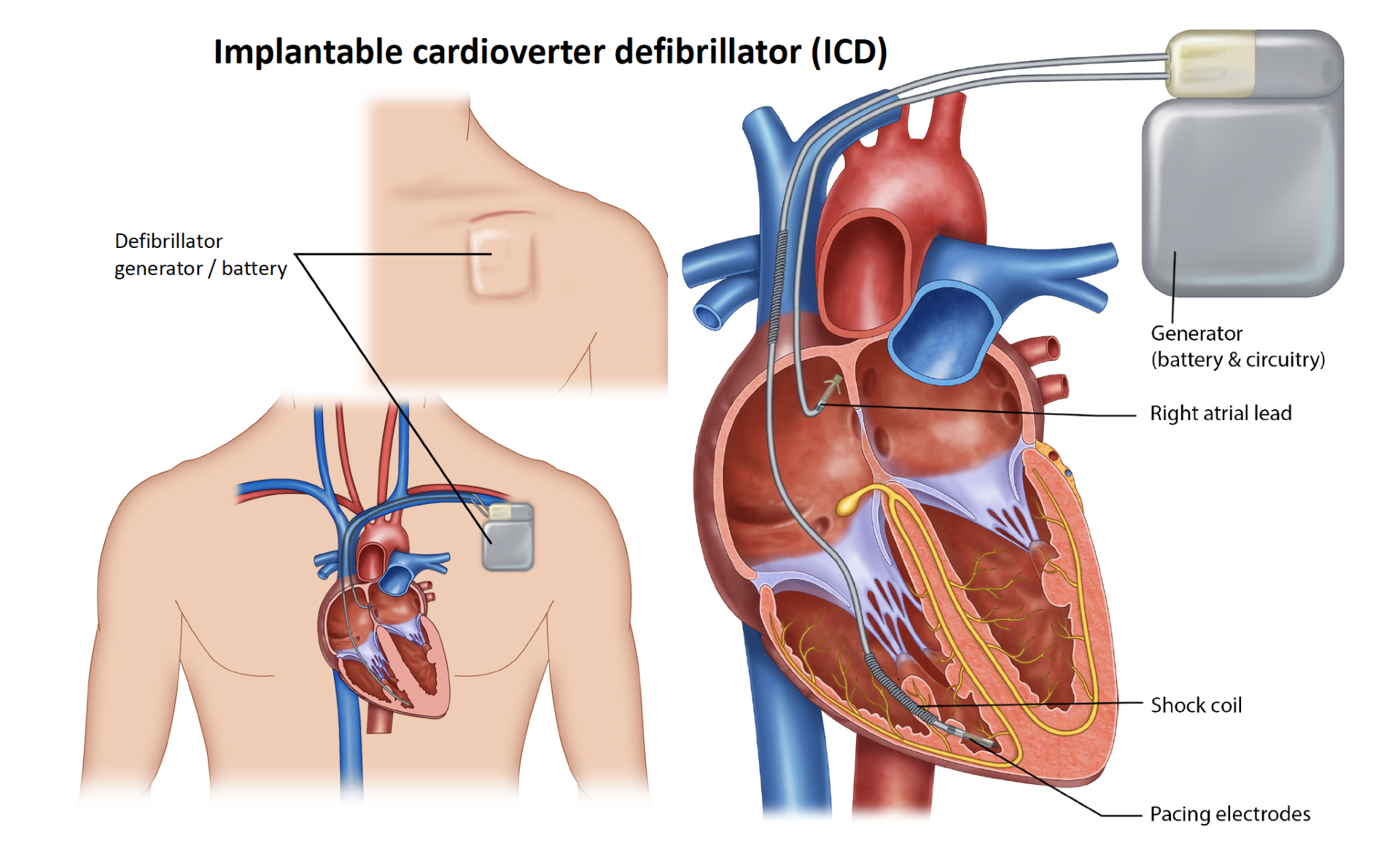
A defibrillator, also called an ICD, is an implantable system comprising of two highly sophisticated parts: lead and a generator (control centre and the battery unit). The device detects, analyses, stimulates and if needed, shocks the heart back to normal rhythm. All standard defibrillators also have a pacemaker function to stop the heart from going too slow. There are special defibrillators such as subcutaneous defibrillators that does not have the pacemaker function. The defibrillator component is always on standby ready to act if sustained dangerous abnormal rhythm is detected. It is designed to stop dangerous abnormal heart rhythms (Ventricular tachycardia; VT and ventricular fibrillation; VF) with a special manoeuvre called anti tachycardia pacing (ATP) or deliver a shock from the inside to reset the rhythm.
The defibrillator wire is usually placed within the heart through veins located just under your collarbone / clavicle. It is usually on left side but can be implanted from the right side as well. The wire(s) are then connected to the generator / battery unit and placed in a space over the chest muscle under the skin. The generator / battery unit is large and does sit prominently in the chest under the collar bone.
Do I need a defibrillator?
The primary purpose of the defibrillator is to protect you from dangerous abnormal rhythms such as sustained ventricular tachycardia (VT) and ventricular fibrillation (VF) that can result in sudden death. In some people, the defibrillator is recommended to prevent sudden death, (Primary prevention). Once you have had sustained VT or VF and survived the event, you are generally recommended to have a defibrillator to prevent another event (secondary prevention).
What are symptoms of ventricular tachycardia (VT) / ventricular fibrillation (VF)?
With VT or VF, you can experience unexpected dizziness, collapse, loss of consciousness and chest pain. People can die suddenly and unexpectedly from VT or VF.
Do defibrillators prevent abnormal rhythms?
No, it is important to understand that defibrillators will not prevent abnormal rhythms. They are an insurance policy. Medications are used to prevent abnormal rhythms. The device will detect fast abnormal rhythm and will deliver therapy to regulate your heart rhythm if it occurs despite medications. You may or may not feel your usual symptoms before you receive therapy from the device. The device acts very quickly but many people may develop symptoms such as loss of consciousness, dizziness or palpitations before the device had delivered therapy.
What is a defibrillation or shock?
A shock has been described by people as a sudden “kick in the chest” which can be painful and distressing. Some people have described it as “startling”, “jolting” and “unsettling”. The feeling is momentary. In very rare cases, people can have repeated shocks in which case, you must attend the local emergency department without delay. Call for help and do not drive. Any person touching you should not be harmed.
Are there different types of defibrillators?
Yes, there a different type of defibrillators. In general defibrillators can have 1, 2 or 3 wires. Most common Is the two-wire system called a dual chamber defibrillator. Instead of using the veins to place these special wires within the heart, in highly selected cases, the wires can be placed outside the heart. This system is called extra vascular or subcutaneous ICD. Different companies manufacture these devices with their own unique offerings. Common defibrillator brands are Medtronic, St Jude Medical, Boston Scientific, Biotronik, Sorin to name a few.
What are the risks of having a defibrillator?
They include but are not limited to the following.
Common risks and complications (more than 5%) include:
- Bruising / bleeding at the pacemaker site
- Large collection of blood (Haematoma) – this can take several weeks to settle
- Pain at the pacemaker site
Uncommon risks and complications (1- 5%) include:
- The pacemaker / device lead(s) can move. The lead will need to be put back into place by repeating this procedure
- Bad bruising if you are taking blood thinning drugs such as Warfarin, Xarelto, Eliquis, Dabigatran Aspirin, Clopidogrel (Plavix or Iscover) or Dipyridamole (Persantin or Asasantin)
- Unexpected device failure. There is a risk of battery (generator) or lead failure. This is uncommon but means the battery or lead will need to be removed and a new one put in
- Infection of the pacemaker site. This will need treatment with antibiotics and/or removal of the pacemaker
Rare risks and complications (less than 1%) include:
- A punctured lung (pneumothorax). This may require a tube to be inserted into the chest to reinflate the lung
- Blood clot in the subclavian vein (Deep vein thrombosis)
- A hole is accidentally made in the heart or heart (perforation) – This will need surgery to repair
- Blood clot in the lung (pulmonary embolus)
- Heart attack
- A stroke. This can cause long term disability
- Death is possible due to the procedure or other heart problems
- Tricuspid regurgitation
- Infection of heart valve and other infections
What happens during the procedure?
ICD insertion is very common and takes approximately 1 hour for a standard dual chamber device. Other special procedures such as CRT can take longer. Procedure is usually performed in the catheter laboratory or operating theatre. You will be lying on a narrow bed under the X-ray machine arm that can move in and out of position.
Pacemakers are generally performed under sedation. General anaesthesia may be considered in some cases and may require an arterial line to monitor your blood pressure. Antibiotics are usually given prior to the procedure.
The upper chest is usually shaved again if needed, cleaned with a special antiseptic wash and once dry, a long sterile drape is placed over the site. The drape covers you from head to toe. You will have someone to assist you if needed. Once you are comfortable, local anaesthetic is administered at the incision site which numbs the area. You’ll feel an initial sharp and burning or pricking sensation when the local anaesthetic is injected but it becomes numb in less than a minute. You may feel a pulling / pushing sensation during the operation which is normal.
A 6 to 9cm cut is made just below your collarbone. The tissue under the skin is carefully dissected and a space is created just above the chest muscle. Usually, a needle is advanced into the vein deeper in the chest under the clavicle. Special dye (Contrast) injection maybe required to identify the vein. The ICD / pacing leads are then guided into the vein and advanced into the correct chamber of your heart using X-ray. They are secured to the heart tissue either by a tiny screw at the end of the wire (Active lead) or soft hooks (Passive lead). The leads are secured to the underlying muscle with permanent sutures over a special cuff on the wire called suture sleeve.
The other end of the lead is connected to the ICD, which is placed in the pocket created over the muscle. The wound is closed with absorbable sutures and a water-resistant dressing applied on top of the wound. In selected cases, we may have to test the function of the defibrillator by delivering a shock through the device at the time of the procedure which will require you to be more sedated / asleep. We may have to induce the dangerous abnormal rhythm to test and ensure that the device if able to respond appropriately. This is not usually required.
You’ll usually need to stay in hospital overnight and may have a chest Xray that night. A pacemaker check is performed the next morning. People can usually go home the next day if tests are all normal.
What happens after a ICD implant?
At the end of your procedure, a simple dressing is applied over the ICD site. You may have a larger dressing applying pressure at the site overnight. You’ll be watched closely in a recovery area, and depending on how you feel, you might need to rest in bed for a while. You will be admitted to the ward for observation overnight with rhythm monitoring. A chest X-ray may be performed in some cases. People are usually discharged the next day after a ICD check.
What happens after discharge?
Wound Care:
- The dressing on your wound should be left in place for two weeks. You may shower, as it is waterproof, but you cannot submerge in a bath or pool.
- Two weeks after the operation, please see your GP to have the dressing removed. Do not remove or change the dressing before this time.
- If the wound becomes red, hot, swollen, more painful or starts to drain fluid, see your local doctor immediately, or call the rooms on 9500-0296.
Special Issues:
- DRIVING: You may drive after two weeks. You cannot hold a commercial driving licence once you have a defibrillator. Every time the device treats an abnormal rhythm either with ATP or a shock there is a driving restriction following the event that can range between a week and 6 months. You can find out more about the driving restrictions from the Austroads website (website: https://austroads.com.au/drivers-and-vehicles/assessing-fitness-to-drive)
- MOVEMENT OF SHOULDER: Please minimise the use of the shoulder on the side of the operation for one month. Do not raise your arm to above shoulder height, do not use the arm to push out of a chair, and no heavy lifting for one month. This is to ensure that the flexible wires connecting the ICD to your heart do not move. After a month these will be firmly stuck in position by the body’s healing process.
- It is normal to take Paracetamol (Panadol) regularly for the first few days at home.
Other Special Issues: As outlined in the information booklet that you would receive from the pacemaker company, these relate to things such as mobile phone use, use of machinery and certain medical tests or procedures you may need in the future, some of which may either interfere with the ICD, or need the ICD to be adjusted beforehand. The device / generator can sometimes move down slightly over time.
IF YOU RECEIVE A SHOCK FROM YOUR DEFIBRILLATOR:
If you are feeling fine, call the rooms the next day. If you have more than one shock, or are feeling unwell afterwards, please go the Emergency Department. By law, you are not permitted to drive a vehicle for one month after receiving a shock from the device.
Airline Travel: You will be given a card with the details of your ICD on it, please keep this in your wallet. A permanent card (resembling a credit card) will be sent to you in about two months. Show this to the security check at the airport, they will search you with a wand rather than walking through the usual metal detector gate.
Follow Up: You will be sent an appointment to see me for an ICD check in 2 -3 months. Usual follow up thereafter is 6-12 monthly appointments to keep track of the device function. It is recommended that you continue your usual follow up with other treating specialists and medical practitioners involved in your care as usual. If you do not receive an appointment, please call the rooms.
Do I have to take it easy once I have an ICD?
Most people with a ICD lead normal active lives, including your normal sexual activities. You can participate in your physical activity after two weeks. Many ICDs allow for increased heart rate when exercising.
What can’t I Do with an ICD? Defibrillators work by detecting electrical signals within your heart. There are external sources of electromagnetic signals that interfere with your device and safest to avoid. The device cannot differentiate between electrical signals from your heart and outside your body. Some examples of activities or situations to avoid include: some types of welding, poorly grounded electrical appliances, and industrial equipment with a large magnetic field. Avoid carrying your mobile phone in your shirt pocket on the same side as your device. In general, people with defibrillators can no longer hold a commercial licence. You will not be allowed to drive a truck, bus or taxi.
How long do ICDs last?
The wires can last for decades but as with most things there is wear and tear over time. The battery lasts about 10 years depending on a few factors. The battery unit is replaced at that time (generator change).
Can I have an MRI scan after an ICD?
Yes, MRI scans can usually be performed with newer ICDs models. There are some exceptions to this rule including abandoned leads and special scenarios. You will have to wait for at least 6 weeks before an MRI scan. Check with your doctor about the details.
Remote monitoring We can monitor the function of your pacemaker while you are at home via remote monitoring. Please refer to the remote monitoring section for more information.
In recommending this procedure your doctor has balanced the benefits and risks of the procedure against the benefits and risks of not proceeding. Your doctor believes there is a net benefit to you going ahead. This is a very complicated assessment.