Atrial fibrillation ablation
Catheter ablation is a highly effective method for managing atrial fibrillation (AF). It has been found that the majority of individuals experience improved symptoms, with success rates estimated to be up to 80%. The burden AF improves significantly following an ablation with improved quality of life. The effectiveness of the procedure can vary based on factors such as the duration of AF, the size of the cardiac chambers, and any existing medical conditions. In some cases, additional ablation procedures may be necessary, with around 30-50% of individuals requiring more than one treatment. Following ablation, many individuals are able to discontinue medications that were previously used to control their heart rhythm. In the vast majority of cases, the frequency of AF episodes significantly decreases and the condition becomes much better managed. Please refer to the catheter ablation section for general information about the admission process and requirements.
What are the risks of having an AF ablation?
They include but are not limited to the following.
Common risks and complications (more than 5%) include:
- Bruising bleeding at the puncture site. Bruising can extend beyond the puncture site and can take a few weeks to improve in some cases.
Uncommon risks and complications (1- 5%) include:
- Development of another arrhythmia
- Bleeding related to the groin puncture site or injury to an artery in the groin. This (rarely) may need surgery and or blood transfusion
- Chest pain / Pericarditis. This is an inflammation of the heart sack that can cause chest pain for some weeks after the procedure and is easily managed with anti-inflammatory medications.
Rare risks and complications (less than 1%) include:
- Fluid around the heart called a “pericardial effusion” which may need to be drained thru a tube under the breast bone or “sternum”
- This may cause long term disability (0.5%)
Heart attack
- Injury to the food pipe related to the ultrasound or temperature probe used during the procedure.
- Injury to the urinary tract if a urinary catheter is required for the procedure.
- Damage to the phrenic nerve that controls the diaphragm (breathing muscle) called phrenic nerve palsy.
- Atrial oesophageal fistula. A hole forms between the oesophagus and the heart. This can cause fever and a stroke as its initial presentation. This may be life threatening.
- Narrowing of the veins from the lungs to the heart called pulmonary vein stenosis. This can be serious, causing breathlessness and may require further procedures
- Damage to normal electrical system requiring a permanent pacemaker
- Death because of this procedure is rare
What happens during an AF ablation?
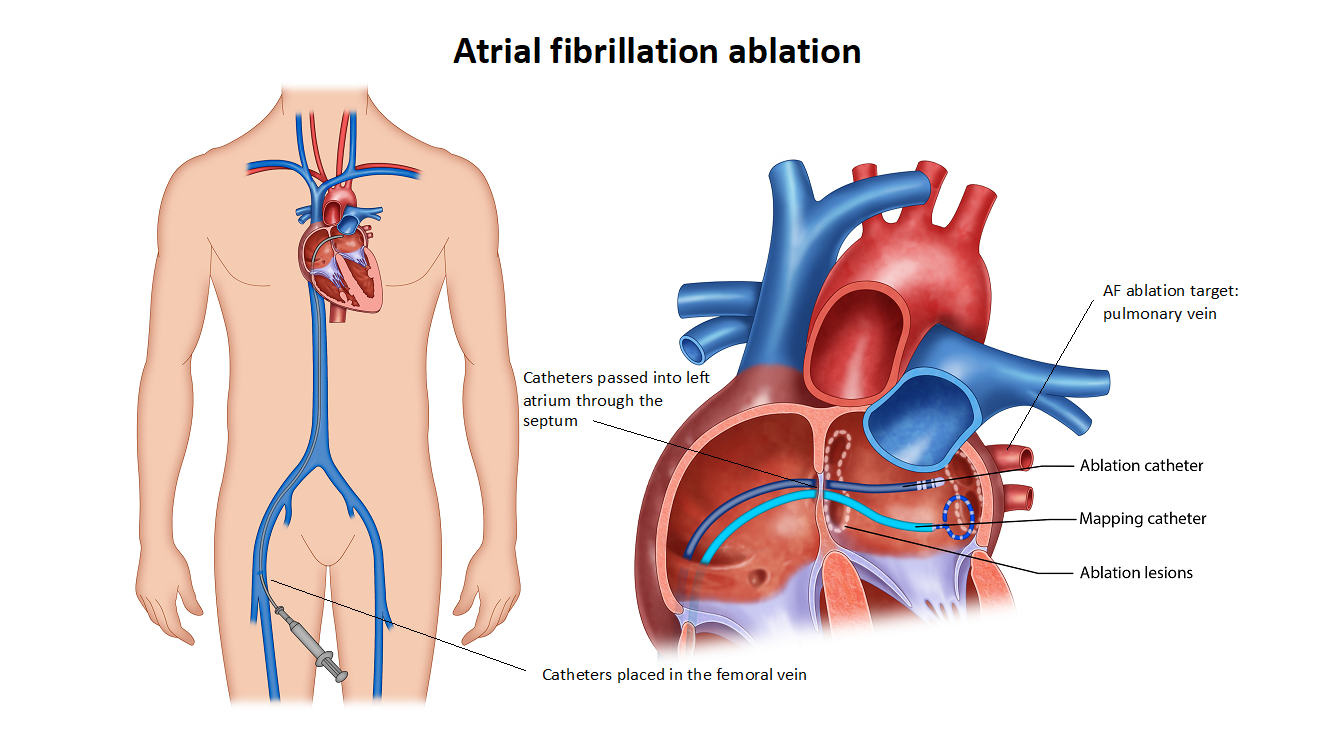
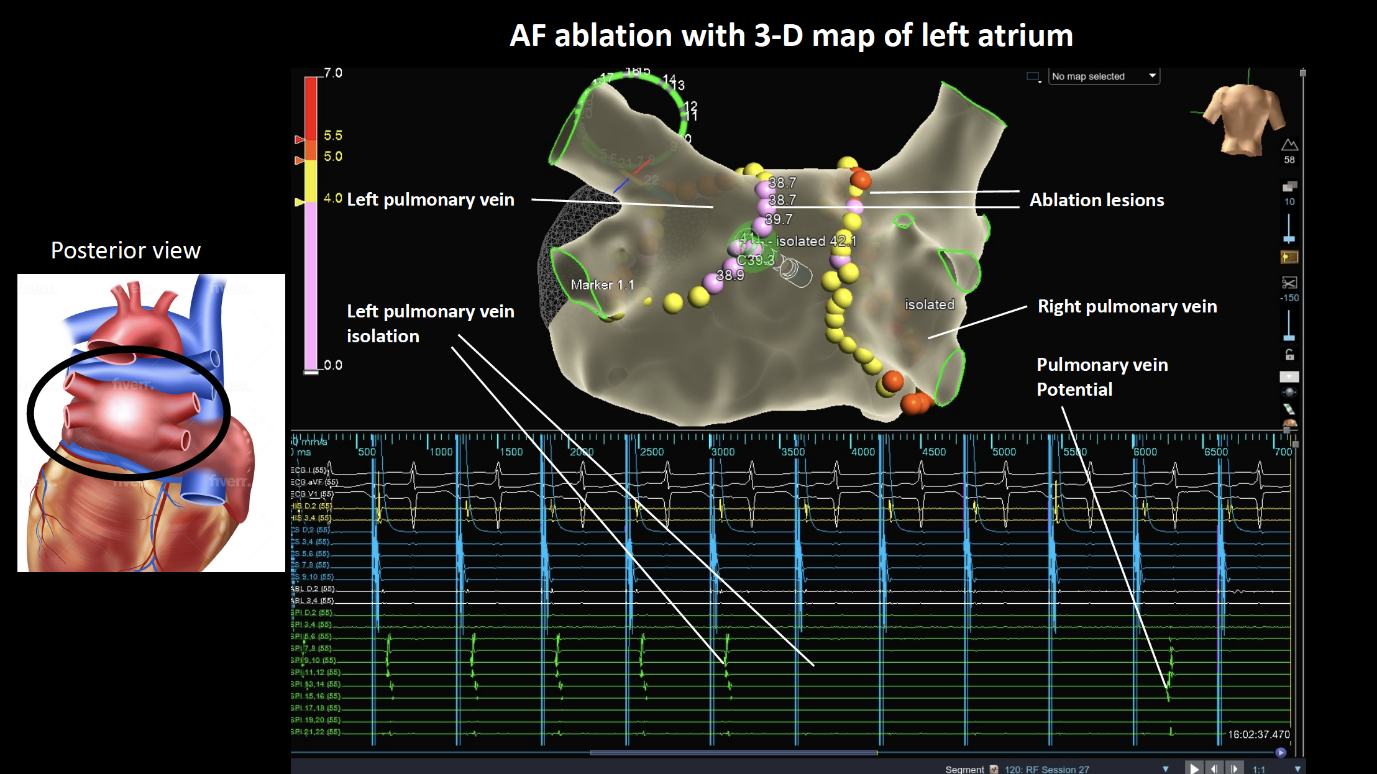
The procedure is typically conducted under general anaesthesia. Several small tubes, about three to four, will be inserted into the femoral vein located on the top of your right thigh. Catheters will be placed through these tubes and advanced up to your heart. To ensure safety, a specialised ultrasound camera known as a transoesophageal echo (TOE) probe will be inserted through your mouth and positioned in the oesophagus next to your heart. This probe serves to assess the presence of any blood clots in the heart before the ablation procedure. If a clot is detected, the procedure will need to be halted. The TOE probe is also utilised to guide the placement of wires across the interatrial septum, a thin membrane that separates the right and left atria. A long needle is used to access the septum. Additional blood thinners are administered to further prevent the risk of stroke. The TOE probe is typically removed, and a temperature probe may be inserted in the oesophagus to monitor temperatures throughout the procedure. A mapping catheter is then advanced into the left atrium to create a three-dimensional model, which helps identify the pulmonary veins and other relevant structures. An ablation catheter is introduced into the left atrium and delivers therapy to create electrical isolation around the pulmonary veins. Depending on the technique used, there may be slight variations. Adenosine, a medication, is often utilized to assess for any remaining abnormal electrical signals. During the procedure, medication or a brief electrical shock (cardioversion) may be administered to control your heart rhythm. The duration of the catheter ablation procedure can range from 2 to 3 hours, or even longer in some cases. In certain instances, unexpected arrhythmias like flutter or supraventricular tachycardia (SVT) may be detected. If necessary, your medical team will proceed with further ablation to avoid the need for a second procedure.

What happens after discharge?
Follow up: An appointment will be made for you to be seen in clinic about 2 months after the procedure. If you do not receive a date for an appointment within 2 weeks, please call the clinic and speak to us.
Medications: Continue your blood thinners / Xarelto / Eliquis / Pradaxa / Warfarin. Your AF medications maybe discontinued after ablation or weaned over 2-3 months. You will usually be prescribed a stomach acid tablet for 1 month.
Post operative care: Driving restriction for 1 week for private vehicle or 4 weeks for commercial vehicle. Avoid strenuous exercise for 2 weeks. Gentle exercise after 1 weeks – e.g. walking.
Return to work: We advise you to take a minimum of 1 week off work, but some people can take up to 2 weeks before you feel strong enough to do more physical tasks.
Symptoms to monitor: It is not uncommon to have a bruise at the groin that extends / spreads after the ablation. This usually resolves over time without any other problems.
It is not uncommon for people to develop some chest pain or headache after ablation that resolves with time.
Bleeding: It is rare to have severe bleeding from the puncture site once you are at home. If bleeding does occur you must: lie flat, apply pressure to the site for 10 minutes. If it continues, call an ambulance for assistance.
Stroke or Fever: If you have an unexpected fever or stroke / mini stroke in the first 1-6 weeks after the procedure, you must attend the local hospital immediately and ask them to contact us.
AF: It is not uncommon to experience AF in the first three months following the ablation which is known as the blanking period. This usually settles. It does not necessarily mean that the procedure has been unsuccessful. If AF recurs and persists for more than 24 hours, please inform the team, we may have to adjust medications or organise a cardioversion
Please contact the rooms if you have any questions or concerns at any time.
In recommending this procedure your doctor has balanced the benefits and risks of the procedure against the benefits and risks of not proceeding. Your doctor believes there is a net benefit to you going ahead. This is a very complicated assessment.