Genetic conditions
Genetic arrhythmic conditions:
Genetic arrhythmic conditions, also known as inherited arrhythmias or hereditary cardiac channelopathies, are a group of disorders that involve abnormalities in the electrical system of the heart. These conditions are caused by genetic mutations that affect the structure or function of ion channels or other proteins involved in the electrical signalling of the heart.
Some examples of genetic arrhythmic conditions include:
Long QT Syndrome (LQTS): LQTS is characterized by prolonged QT intervals on an electrocardiogram (ECG), which can lead to life-threatening arrhythmias such as torsades de pointes and sudden cardiac arrest.
Brugada Syndrome (BrS): BrS is characterized by specific ECG patterns and an increased risk of ventricular arrhythmias and sudden cardiac death, particularly during sleep.
Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT): CPVT is a condition in which exercise or emotional stress can trigger life-threatening ventricular tachycardia, potentially leading to sudden cardiac arrest.
Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy (ARVD/C): ARVD/C is a condition in which the normal myocardial tissue of the right ventricle is gradually replaced by fatty or fibrous tissue, leading to arrhythmias and, in some cases, heart failure.
These genetic arrhythmic conditions can have variable penetrance, meaning that not all individuals with the genetic mutation will necessarily develop symptoms or experience arrhythmias. However, individuals with a family history of these conditions or concerning symptoms may undergo genetic testing and evaluation by a cardiologist specializing in cardiac electrophysiology to assess their risk and guide appropriate management and treatment options.
What is a genetic disorder?
A genetic disorder is a health condition or disease that is caused by abnormalities or mutations in an individual’s genes or chromosomes. Genes are segments of DNA that contain instructions for the development, functioning, and regulation of our bodies. Genetic disorders can be inherited from one or both parents or can occur spontaneously due to new mutations in the genes.
How do I know if I have a genetic disorder?
Individuals who are suspected of having an inherited arrhythmia condition are typically referred to a specialised clinic focused on cardiovascular genetics for genetic testing. Genetic testing plays a crucial role in identifying potential genetic disorders that may require intervention. By undergoing genetic testing, we can assess your specific risks and provide appropriate recommendations to prevent complications for both you and your family.
It’s important to note that not all individuals with the condition will have detectable genetic abnormalities. However, in cases where a specific mutation (known as a pathogenic mutation) is identified, it may be advisable for your family members to undergo cascade screening to determine their own risks of the condition.
Genetic testing carries implications for various aspects of your future, including insurance coverage, family planning, and participation in competitive sports. To ensure comprehensive support, a genetic counsellor is typically involved as part of the cardio-genetics clinic. They can provide guidance, information, and address any concerns or questions you may have throughout the genetic testing process.
Why are these genetic disorders of clinical concern?
The clinical impact of these genetic disorders varies and is unique to each specific condition.
Long QT syndrome:
What is Long QT syndrome (LQTS)?
The QT segment is referred to as the relaxation phase.
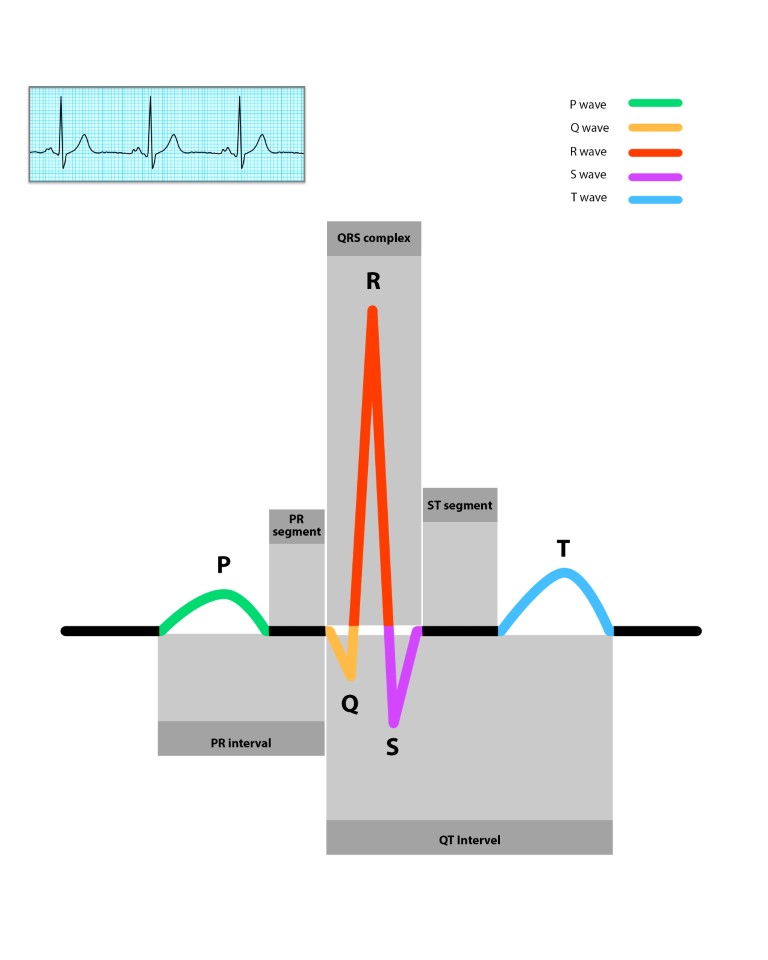
This is the time it takes for the heart to reset after each contraction. The corrected QT (QTc) is usually less than 0.46seconds / 460milliseconds (ms). Women tend to have slightly longer QTc. This segment can also be prolonged due to common medications.
Genetic disorders can affect the QT segments which is termed Long QT syndrome or LQTS. There are numerous subtypes but LQTS 1, 2 and 3 are the most common with important clinical manifestations.
LQTS type 1: Mutation involving KCNQ1 – related to Potassium ion channels. Emotional stress or exercise, particularly swimming, has been known to cause abnormal rhythms.
LQTS type 2: Mutation involving KCNH2 – related to Potassium ion channels. Emotional stress, surprise and startling can trigger abnormal rhythms.
LQTS type 3: Mutation involving SCN5A – related to Sodium channel abnormality. Arrhythmia occurs during sleep or rest.
Why is LQTS relevant?
Inherited arrhythmic conditions such as LQTS can lead to abnormal heart rhythms that can results in loss of consciousness or sudden death.
What are the treatment options for LQTS?
Treatment will vary significantly between people based on their type of LQTS, presentation, severity, and genetic abnormality. Long-acting beta blockers are considered mainstay of treatment in LQTS 1 & 2. Flecainide is often considered for LQTS 3. Genetic treatments may possible in the near future for specific subtypes.
What are some general recommendations and treatment for patients with LQTS?
Here are some important lifestyle recommendations for individuals with Long QT syndrome (LQTS):
Avoid medications that can prolong the QT interval. It is crucial to inform your doctors about your LQTS condition before taking any prescribed medications. The “qtdrugs” website offers an updated list of medications that should be avoided in LQTS.
Medications: The main treatment for LQTS types 1 and 2 is beta blockers.
Consideration of implantable cardioverter-defibrillators (ICDs) in individuals who have survived a cardiac arrest or are deemed to be at high risk of experiencing cardiac arrest.
Left cervical sympathectomy may be considered in highly selected cases.
These recommendations aim to minimise the risk of arrhythmias and potential life-threatening events associated with LQTS.
What are some useful resources for LQTS?
- www.qtdrugs.orgProvides a list of medications to be avoided in Long QT syndrome
- www.cidg.org(Cardiac Inherited Disease Group, New Zealand)
BRUGADA SYNDROME:
What is Brugada syndrome (BrS)?
Brugada syndrome is a genetic cardiac condition that is characterized by specific abnormalities seen on a 12-lead ECG. These abnormalities include a distinctive coved-shaped pattern in the ST segment, an atypical right bundle branch block pattern, and a risk of developing ventricular arrhythmias that can lead to sudden cardiac death. It is important to note that many individuals with Brugada syndrome may not experience any symptoms and may be unaware of their condition. Some individuals may exhibit the ECG changes associated with Brugada syndrome without experiencing any clinical events or abnormal heart rhythms. This ECG pattern is referred to as the Brugada pattern.
Why is BrS relevant?
Inherited arrhythmic conditions can lead to abnormal heart rhythms that can result in loss of consciousness or sudden death. It has implications to your family.
What are some general recommendations and treatment for patients with Brugada pattern on ECG or BrS?
Some important lifestyle recommendations for patients with BrS include the following:
Avoid medications that can worsen BrS. Before you take any prescribed medications, please inform your doctors about your condition. The “brugadadrugs” website provides a constantly updated list of medications to be avoided in BrS.
Aggressive treatment and avoidance of fever. Treat infections early and take paracetamol regularly in the event of common infections.
Implantable cardioverter defibrillators in those who have survived a cardiac arrest or in those considered as high risk of having cardiac arrest
Medications such as quinidine is very effective in BrS but is difficult to source
Useful resources for BrS:
- brugadadrugs.org Provides a list of medications to be avoided in BrS
- https://www.csanz.edu.au/documents/guidelines/clinical_practice/Brugada_Syndrome.pdf CSANZ Brudaga information sheet