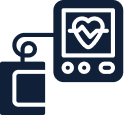
Atrial fibrillation ablation
Catheter ablation for AF is an effective way to control your heart rhythm. Most people are symptomatically better with success estimated at up to 80% depending on factors such as duration of AF, size of cardiac chambers and comorbidities. 30-50% of people may need to have more than one procedure in time as the heart may heal at sites of prior ablation or new areas may appear. Often medications used to control the heart rhythm can be stopped following ablation. In the vast majority, amount of AF after ablation is markedly reduced and much better controlled.
What are the risks of having an AF ablation?
They include but are not limited to the following.
Uncommon complications (1- 5%) include:
- Development of another arrhythmia
- Bleeding related to the groin puncture site or injury to an artery in the groin. This (rarely) may need surgery and or blood transfusion
- Chest pain / Pericarditis. This is an inflammation of the heart sack that can cause chest pain after the procedure and is easily managed with anti inflammatories
Rare risks and complications (less than 1%) include:
- Fluid around the heart called a “pericardial effusion” which may need to be drained thru a tube under the breast bone or “sternum”
- A stroke. This may cause long term disability (0.5%)
- Requirement for a pacemaker following the procedure
- Injury to the food pipe related to the ultrasound or temperature probe used during the procedure.
- Damage to the phrenic nerve that controls the diaphragm (breathing muscle) called phrenic nerve palsy.
- Atrial oesophageal fistula. A hole forms between the gullet and heart. This can cause vomiting of blood and a stroke. This may be life threatening.
- Narrowing of the veins from the lungs to the heart called pulmonary vein stenosis.
- Damage to normal electrical system requiring a permanent pacemaker
- Death because of this procedure is rare
What are the costs involved with an ablation?
If you are having this procedure in a public hospital as a public patient, the cost is covered by Medicare. If you are having this procedure in a private hospital, there is no additional out of pocket cost for our specialists. The usual hospital excess applies. Anaesthetists often have an out-of-pocket cost that we encourage you to discuss prior to your planned procedure.
How do I prepare for an ablation?
You will receive a letter with instructions and steps required prior to your procedure including, date of admission, fasting instructions, medications to stop and items to bring with you. You will usually need recent blood test for your kidneys and blood count prior. In general, do not eat or drink for 6 hours before your procedure. Ask your doctor about taking your usual medications. Blood thinners are usually continued for AF ablation procedure. If you take SGLT2 medicine for heart failure or diabetes, you will need to stop taking them at least 3 days before your surgery. Leave any personal items of value such as jewellery at home.
What happens when you arrive at the hospital?
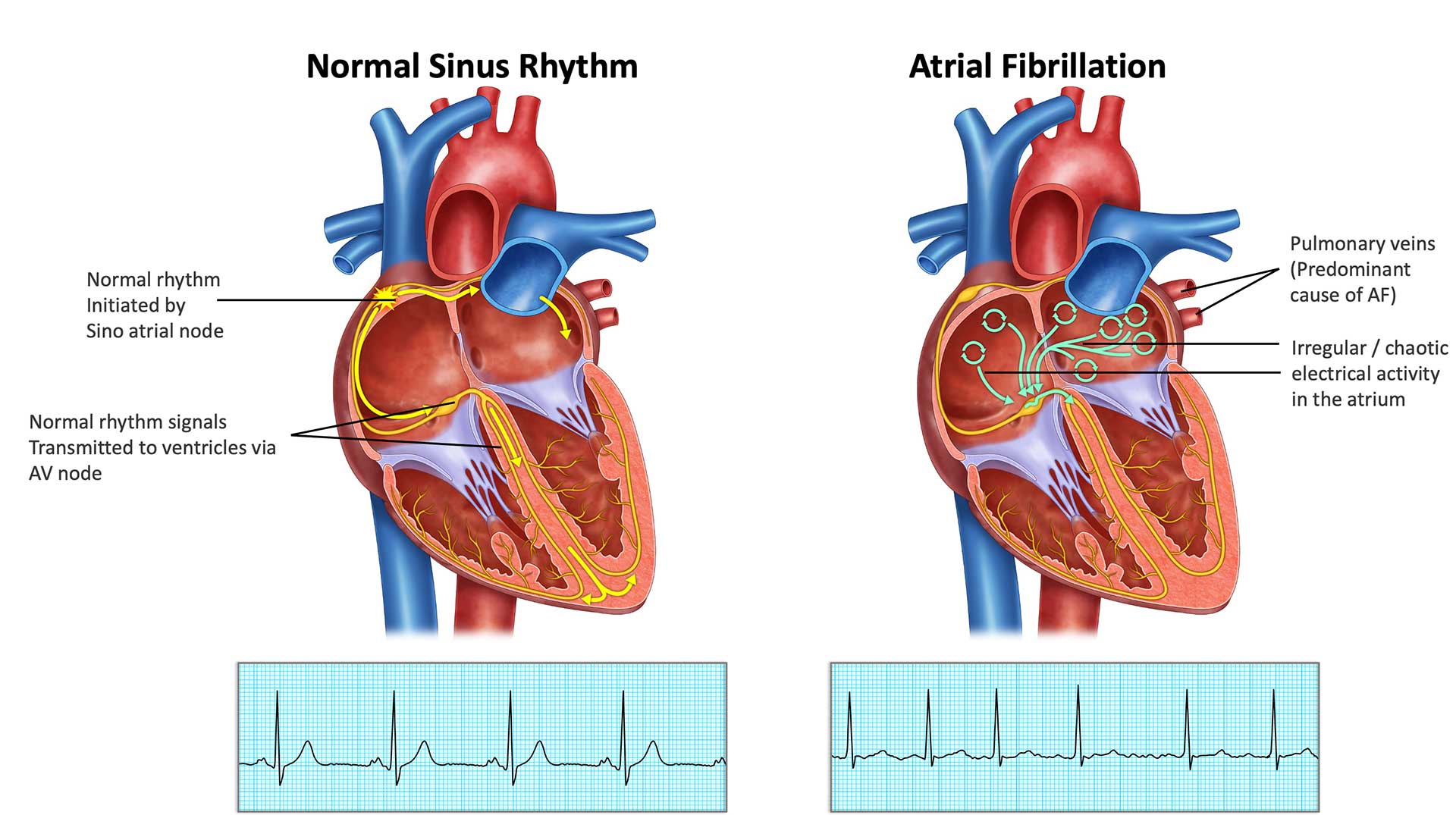
Once you arrive at the hospital for your procedure, you will usually be directed to the cardiac catheter laboratory admission area where you will be formally admitted as a hospital patient. You will be asked to change into hospital gown and put away all your valuable belongings. You will have some basic tests such as ECG, have your vitals recorded, groin shaved and have a cannula inserted into your arm to assist with the procedure. The technologists will place special stickers and wires on your chest and back. In most cases a pre ablation cardiac CT scan of the heart is performed to guide the ablation procedure. If you have this performed externally, please ensure you ask for a copy of the CD to the hospital with you.
Ablation will be performed under general anaesthesia which requires an anaesthetist. The anaesthetist will speak with you about their role. You will require an arterial line to monitor your blood pressure during the ablation that carries some risk of complications.
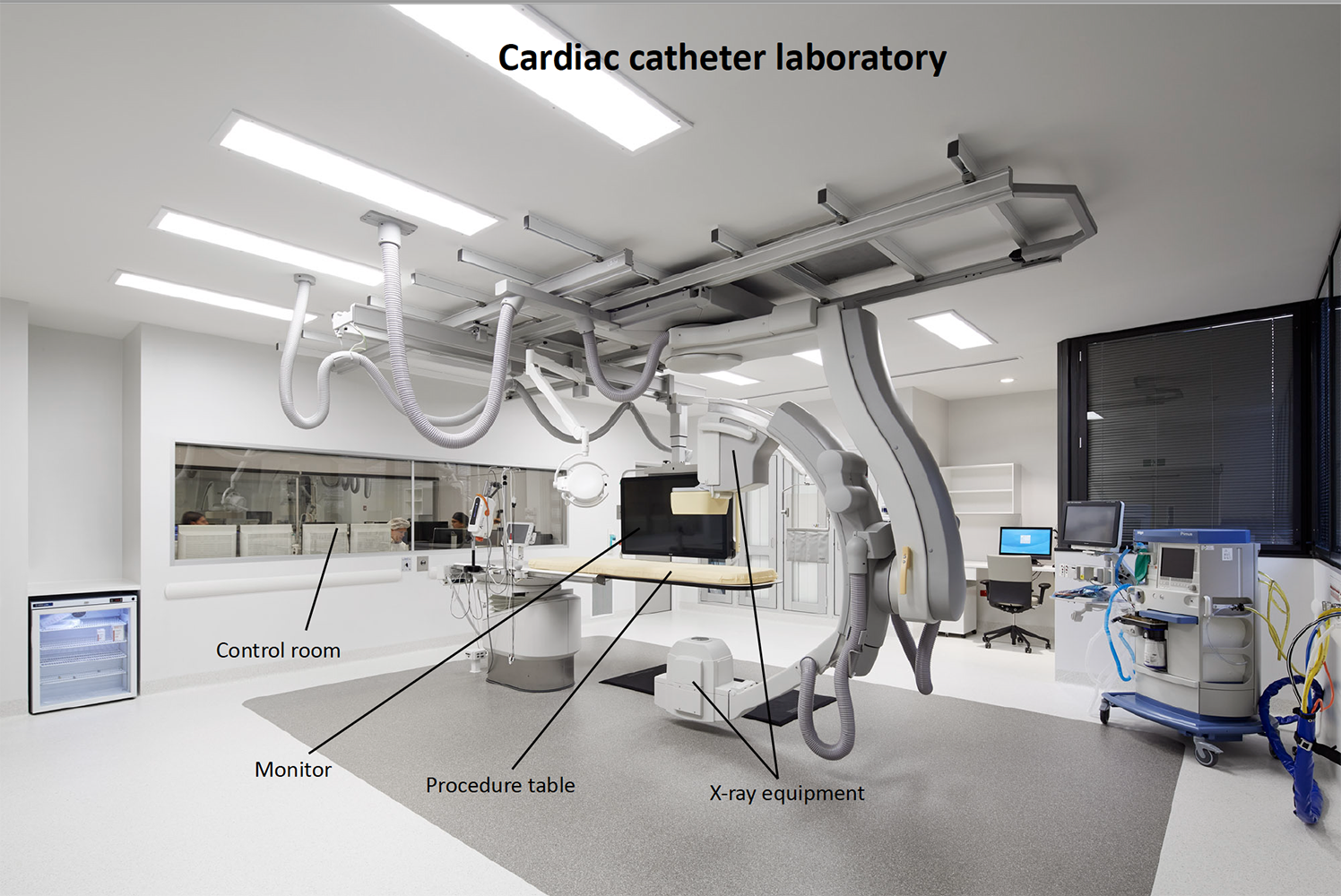
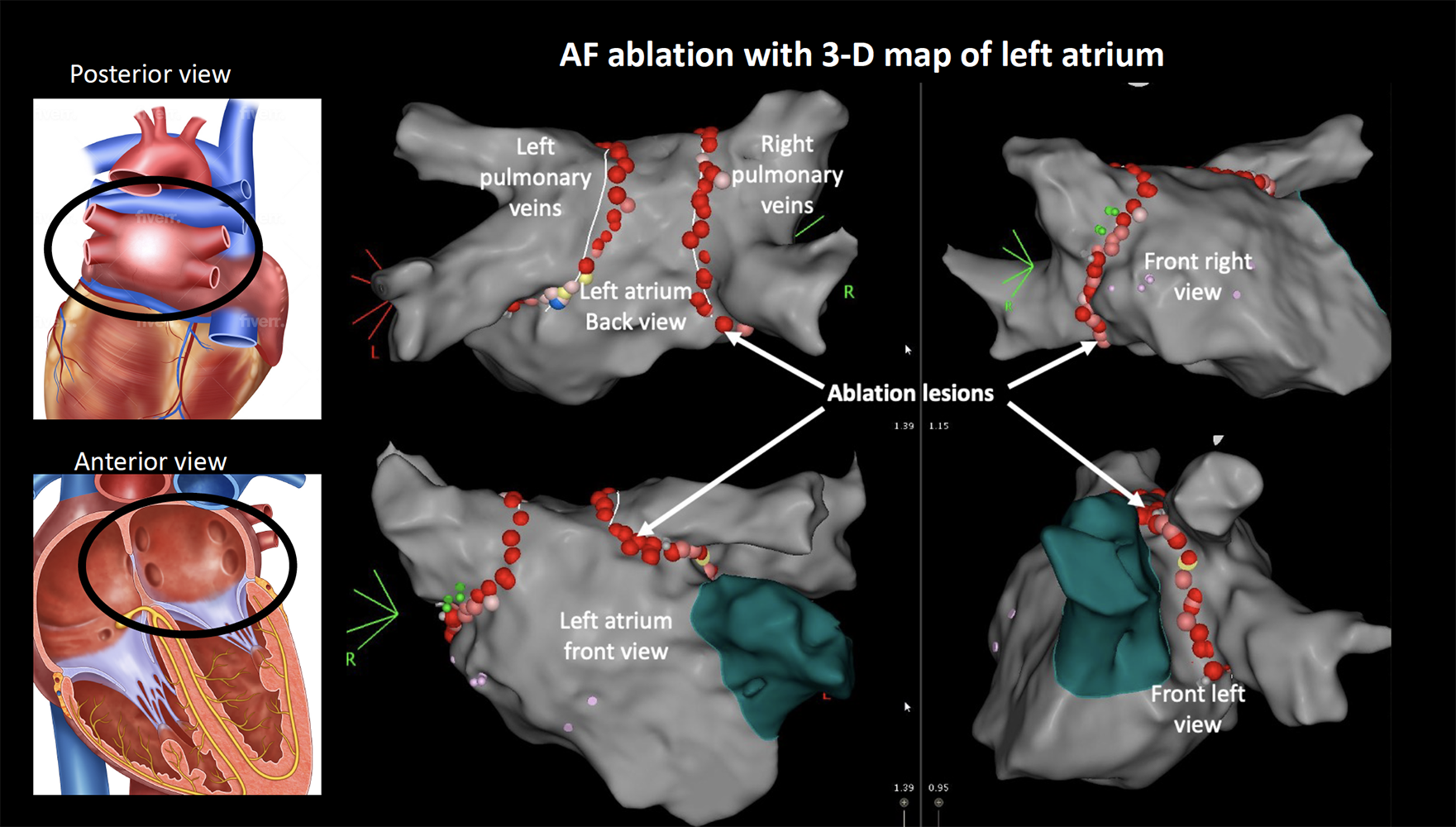
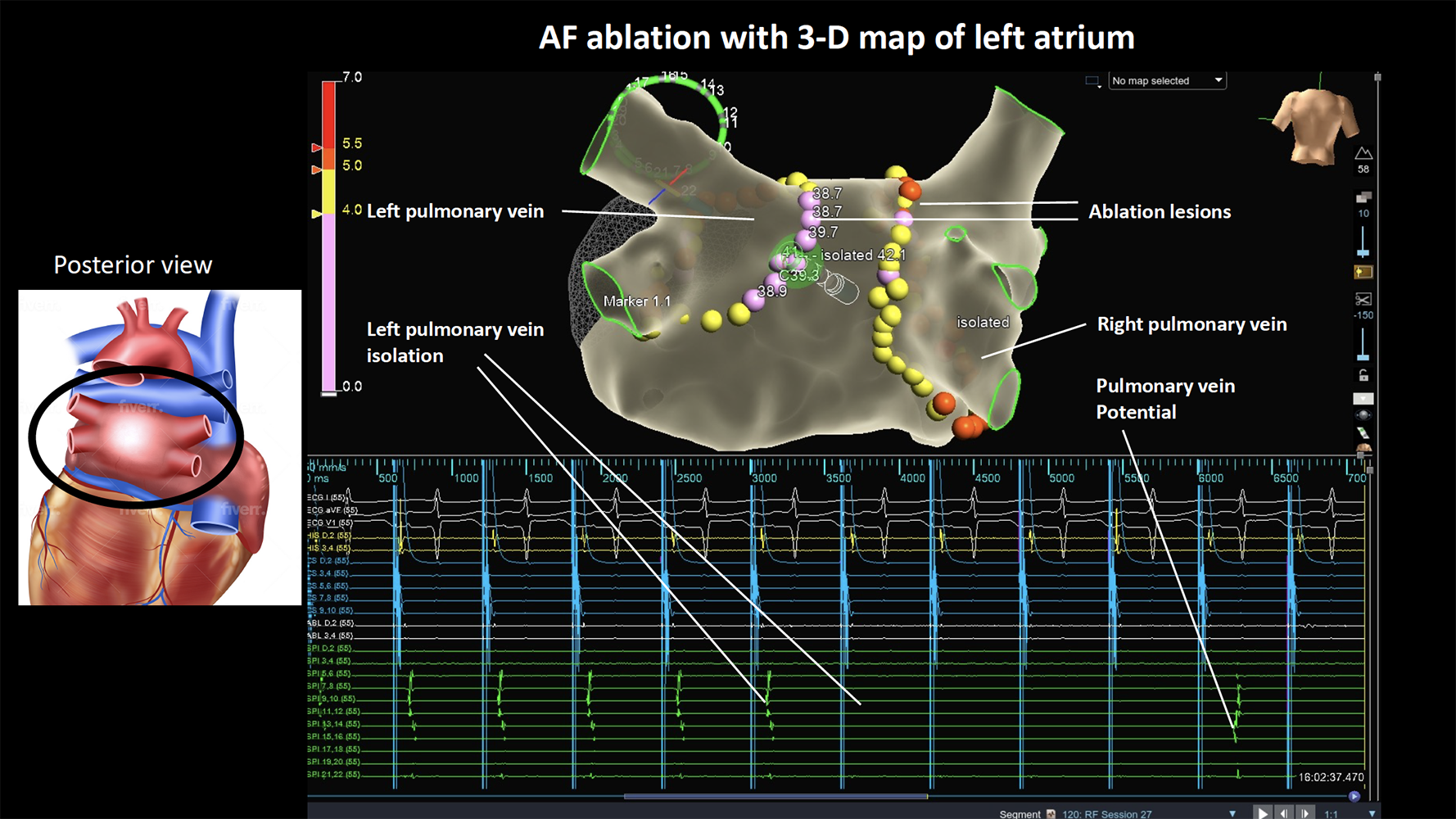
You will be transferred to the catheter laboratory and will have to lie on a narrow hard bed under the X-ray machine. The anaesthetist will get you off to sleep (general anaesthesia). Local anaesthetic is administered at the groin which numbs the area. Four small tubes called sheaths are passed into the vein in the right groin through which catheters are inserted and gently passed up until they reach your heart. An X-ray machine guides the catheters to your heart. A special ultrasound camera called a transoesophageal echo (TOE) probe is advanced through your mouth into your oesophagus (gullet) that sits next to your heart. This is used to check for any clots in the heart prior to ablation. If a clot is found, the procedure will have to be abandoned. The TOE is also used to guide the wires across from the right side to the left atrium (LA) through a thin membrane called the interatrial septum. A long needle is used to get access across the septum. Additional blood thinners are given to thin the blood further to prevent a stroke. The TOE probe is usually removed, and a temperature probe usually placed in the oesophagus to monitor for any high temperatures throughout the procedure. A mapping catheter is advanced into the LA to make a 3-D model which identifies the pulmonary veins and other structures of relevance. An ablation catheter is advanced into the left atrium that applies the radiofrequency energy around the pulmonary veins to electrically isolate those veins. Medication called adenosine is often used to check for any areas of persisting signals. You may need medication or a brief shock to control your rhythm during the procedure. The catheter ablation procedure can take 2 -3 hrs or more in some cases. In some cases, additional unexpected rhythms such as flutter or SVT becomes apparent. Your doctors will proceed to further ablation if required to prevent you having to return for a second procedure.
What happens after an ablation?
At the end of your procedure, your doctor will remove the catheters and apply pressure, followed by a simple dressing. You may have a little device applying pressure at the puncture site for a few hours. You’ll be watched closely in a recovery area, and depending on how you feel, you might need to rest in bed for a while. You will be admitted to the ward for observation overnight with rhythm monitoring. You are generally required to lay flat on your back for about 4 hours after your procedure. People are usually discharged the next day.
What happens after discharge?
Follow up: An appointment will be made for you to be seen in clinic about 2 months after the procedure. If you do not receive a date for an appointment within 2 weeks, please call the clinic and speak to us.
Medications: Continue your blood thinners / Xarelto / Eliquis / Pradaxa / Warfarin. Your AF medications maybe discontinued after ablation or weaned over 2-3 months. You will usually be prescribed a stomach acid tablet for 1 month.
Post operative care: Driving restriction for 1 week for private vehicle or 4 weeks for commercial vehicle. Avoid strenuous exercise for 2 weeks. Gentle exercise after 1 weeks – e.g. walking.
Return to work: We advise you to take a minimum of 1 week off work, but some people can take up to 2 weeks before you feel strong enough to do more physical tasks.
Symptoms to monitor: It is not uncommon to have a bruise at the groin that extends / spreads after the ablation. This usually resolves over time without any other problems.
It is not uncommon for people to develop some chest pain or headache after ablation that resolves with time.
Bleeding: It is rare to have severe bleeding from the puncture site once you are at home. If bleeding does occur you must: lie flat, apply pressure to the site for 10 minutes. If it continues, call an ambulance for assistance.
Stroke or Fever: If you have an unexpected fever or stroke / mini stroke in the first 1-6 weeks after the procedure, you must attend the local hospital immediately and ask them to contact us.
AF: It is not uncommon to experience AF in the first three months following the ablation which is known as the blanking period. This usually settles. It does not necessarily mean that the procedure has been unsuccessful. If AF recurs and persists for more than 24 hours, please inform the team, we may have to adjust medications or organise a cardioversion
Please contact the rooms if you have any questions or concerns at any time.
In recommending this procedure your doctor has balanced the benefits and risks of the procedure against the benefits and risks of not proceeding. Your doctor believes there is a net benefit to you going ahead. This is a very complicated assessment.
Download the AF patient information sheet {link to AF information sheet}
Signature of patient: Date: