Catheter ablation
What is an ablation / catheter ablation?
An ablation, specifically catheter ablation, is a medical procedure used to treat certain heart rhythm disorders, also known as arrhythmias. It is a minimally invasive procedure performed by a specialised cardiologist called an electrophysiologist.
During a catheter ablation, thin, flexible tubes called catheters are inserted into blood vessels, usually in the groin area, and threaded up to the heart. These catheters have electrode tips that can deliver various forms of energy, such as radiofrequency energy or cryotherapy (extreme cold) or PFA, to the specific areas of the heart that are causing the abnormal electrical signals responsible for the arrhythmia.
The purpose of the ablation is to target and destroy the abnormal tissue or pathways in the heart that are causing the arrhythmia. This is achieved by delivering the energy to the precise locations identified by mapping the heart’s electrical signals during the procedure. By ablating or eliminating the abnormal tissue, the goal is to restore the heart’s normal rhythm.
Catheter ablation is commonly used to treat arrhythmias such as atrial fibrillation, atrial flutter, supraventricular tachycardia, and certain types of ventricular tachycardia. The specific type of ablation and the techniques used depend on the type and location of the arrhythmia being treated.
It’s important to note that catheter ablation is a specialised procedure that requires careful evaluation and consideration by an electrophysiologist. The decision to undergo ablation depends on several factors, including the severity of the arrhythmia, the impact on the patient’s quality of life, and the potential risks and benefits of the procedure.
How do you get to the heart?
Ablation is a minimally invasive procedure that involves the use of a thin, long catheter, typically measuring a few millimeters in width. Your specialist will guide and manipulate the catheter using a handle at the other end. The catheter is inserted through a vein, usually located at the top of your right leg, and carefully advanced up to the heart with the help of X-ray imaging for guidance. In certain situations, the catheter may need to be placed in the artery of the right leg or the vein of the left leg.

Are there any advantages between the cold, hot and PFA ablation types?
There are some differences between the modalities of ablation. They have their own pros and cons that you can discuss with your treating doctor if required.
Why do I need a catheter ablation?
You doctor(s) may recommend a catheter ablation as a treatment for abnormal heart rhythms such as atrial fibrillation, atrial flutter, supraventricular tachycardia, premature ventricular contractions, and ventricular tachycardia.
Can you have more than one ablation procedure?
Yes, it is not uncommon to have more than one ablation procedure. It depends on the type of arrhythmia and planned procedure. Some arrhythmias, such as atrial fibrillation, commonly require more than one ablation procedure. Whereas AV node and AVNRT (SVT) ablations are highly effective and are expected to be >98% effective. People can also develop different types of arrhythmia overtime requiring more than one ablation procedure for the respective conditions.
What are the risks of having a catheter ablation?
While serious risks are unlikely, there are risks associated with a catheter ablation procedure. The risks will depend on the type of ablation planned, the vessel we need to access and the chamber in the heart that requires attention.
In general, the most common risk for this procedure is bruising or swelling at the puncture site in the leg.
Less common complications are:
⦁ Abnormal heart rhythms, called arrhythmias because of ablation
⦁ Inflammation of the heart lining called pericarditis
⦁ Major bleeding or bruising at the puncture site requiring transfusion or surgery
⦁ Infection
⦁ Damaged heart muscle, heart valves or blood vessels that may require surgery
⦁ Blood clot in the lung or legs
⦁ Stroke or heart attack
⦁ Death from this procedure is exceedingly rare
Your doctor will have a more detailed discussion about risks before you agree to the surgery. As there are many different forms of catheter ablation, it’s important you take the time to discuss your procedure with your doctor and raise any questions or concerns. Your doctor will ask you to sign a consent form to agree to the procedure.
What are the costs involved with an ablation?
If you are having this procedure in a public hospital as a public patient, the cost is covered by Medicare. If you are having this procedure in a private hospital, there is usually no additional out of pocket cost for our specialists. The usual hospital excess applies. In general, anaesthetists have an out-of-pocket cost that we encourage you to discuss prior to your planned procedure.
How do I prepare for an ablation?
You will receive a letter with instructions and steps required prior to your procedure including, date of admission, fasting instructions, medications to stop and items to bring with you.
In General:
⦁ Do not eat or drink for 6 hours before your procedure.
⦁ Ask your doctor about taking your usual medications. If you take SGLT2 medicine for heart failure or diabetes, you will need to stop taking them at least 3 days before your surgery. Your procedure may be cancelled on the day of surgery if you had taken this medication. If you take some Semaglutide (Ozempic) or Liraglutide (Victoza, Saxenda), these will have to be stopped atleast 1 week prior.
⦁ Leave any personal items of value such as jewellery at home
⦁ Blood thinners are usually continued for ablation procedures except for some type of PVC and VT ablations.
⦁ You will usually need recent blood test for your kidneys and blood count prior
What happens during an ablation?
Once you arrive at the hospital for your procedure, you will usually be directed to the cardiac catheter laboratory admission area where you will be formally admitted as a hospital patient. You will be asked to change into hospital gown and put away all your valuable belongings. You will have some basic tests such as ECG, have your vitals recorded, groin shaved and have a cannula inserted into your arm. Some procedures are performed under general anaesthesia and requires an anaesthetist. If so, the anaesthetist will speak with you about their role. Many patients require an arterial line to monitor your blood pressure during the ablation that carries some risk of complications. Your anaesthetist will speak to you about this if required.
You may have to wait for several hours before your procedure, we suggest bringing a good book. Your catheter ablation procedure takes place in the catheter laboratory which looks like an operating theatre.
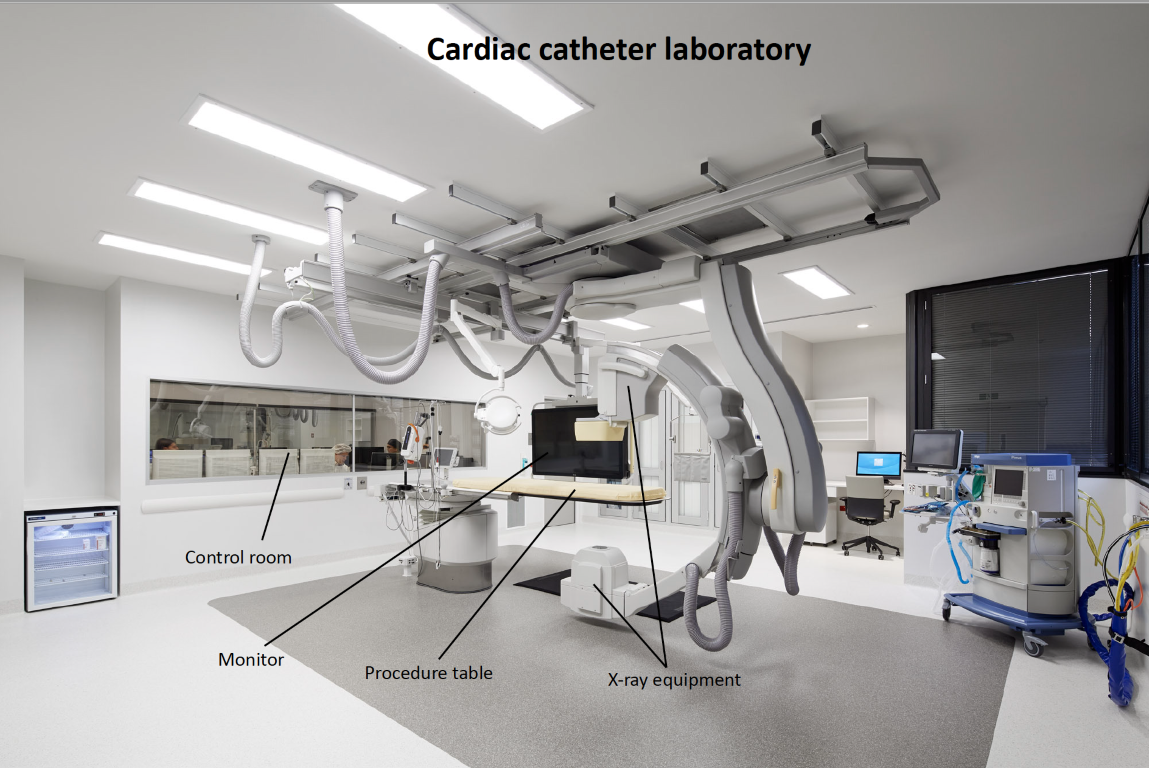
You will either walk or will be taken to the procedure room on a trolley and be asked to lie on the procedure table. Some procedures are performed under sedation. In these cases, you will be awake during your procedure but before it begins your doctor will give you sedating medications to help you remain calm and relaxed. This is given through a cannula in your arm.
During the procedure:
⦁ Local anaesthetic is administered which numbs the area where the needles and tube are placed
⦁ Through a tube (sheath), catheters are inserted into the groin and gently passed through veins (or artery) until they reach your heart
⦁ An X-ray machine guides the catheters to your heart
⦁ Electrical impulses are used to make your heart beat at different speeds to study the heart
⦁ You may need medication to control your heartbeat during the procedure
⦁ Your heart beat and rhythm will be recorded using sophisticated equipment
The exact location of your arrhythmia is determined using a technique called ‘mapping’. The ablation catheter is then placed at the area of interest and energy applied to eliminate the source of the abnormal electrical activity to correct those abnormal heartbeats. The catheter ablation procedure can take between 1 and 4hrs or more in some cases. Make sure you let your doctor know if you experience any discomfort or pressure in your chest at any time during the procedure.
What happens after an ablation?
At the end of your procedure, your doctor will remove the catheters and apply pressure, followed by a dressing where the catheters were placed. You may have a little device applying pressure at the puncture site for a few hours. You’ll be watched closely in a recovery area, and depending on how you feel, you might need to rest in bed for a few hours. You are generally required to lay flat on your back for about 4 hours after your procedure. Most people can return to their normal activities in a few days to two weeks depending on the procedure. For two or three days after your catheter ablation you may feel tired, sore in your chest and leg (where the catheters were placed) or experience fast, irregular or skipped heartbeats. Your doctor may change your usual heart medication.
Follow up:
⦁ An appointment will be made for you to be seen in clinic about 2 months after the procedure.
⦁ If you do not receive a date for an appointment within 8 weeks, please call the clinic and ask to speak to the secretary.
Medications:
⦁ If you are on blood thinners, continue them: Xeralto / Eliquis / Pradaxa / Warfarin
⦁ Your other heart rhythm medications maybe discontinued following ablation or weaned after 2-3 months
⦁ You may be prescribed a stomach acid tablet for 1 month
Post operative care:
⦁ Driving restriction for up to 1 week (Private vehicle) or 4 weeks for commercial vehicle
⦁ Avoid strenuous exercise for 2 weeks
⦁ Gentle exercise after 1 weeks – e.g., long walks.
⦁ Return to work: We advise you to take a minimum of 1 week off work, but some people can take up to 2 weeks before you feel strong enough to do more physical tasks.
Symptoms to monitor:
⦁ It is not uncommon to have a bruise at the groin that extends / spreads after the ablation. This usually resolves over a few weeks without any other problems. If it becomes increasingly painful or swollen, seek medical attention.
⦁ Bleeding: It is rare to have severe bleeding from the puncture site once you are at home. If bleeding does occur you must: lie flat, apply pressure to the site for 10 minutes. If it continues, call an ambulance for assistance.
Please contact our rooms if you have any questions or concerns at any time. We are happy to hear from you if you have any questions or concerns.