Atrial fibrillation (AF)
What is AF?
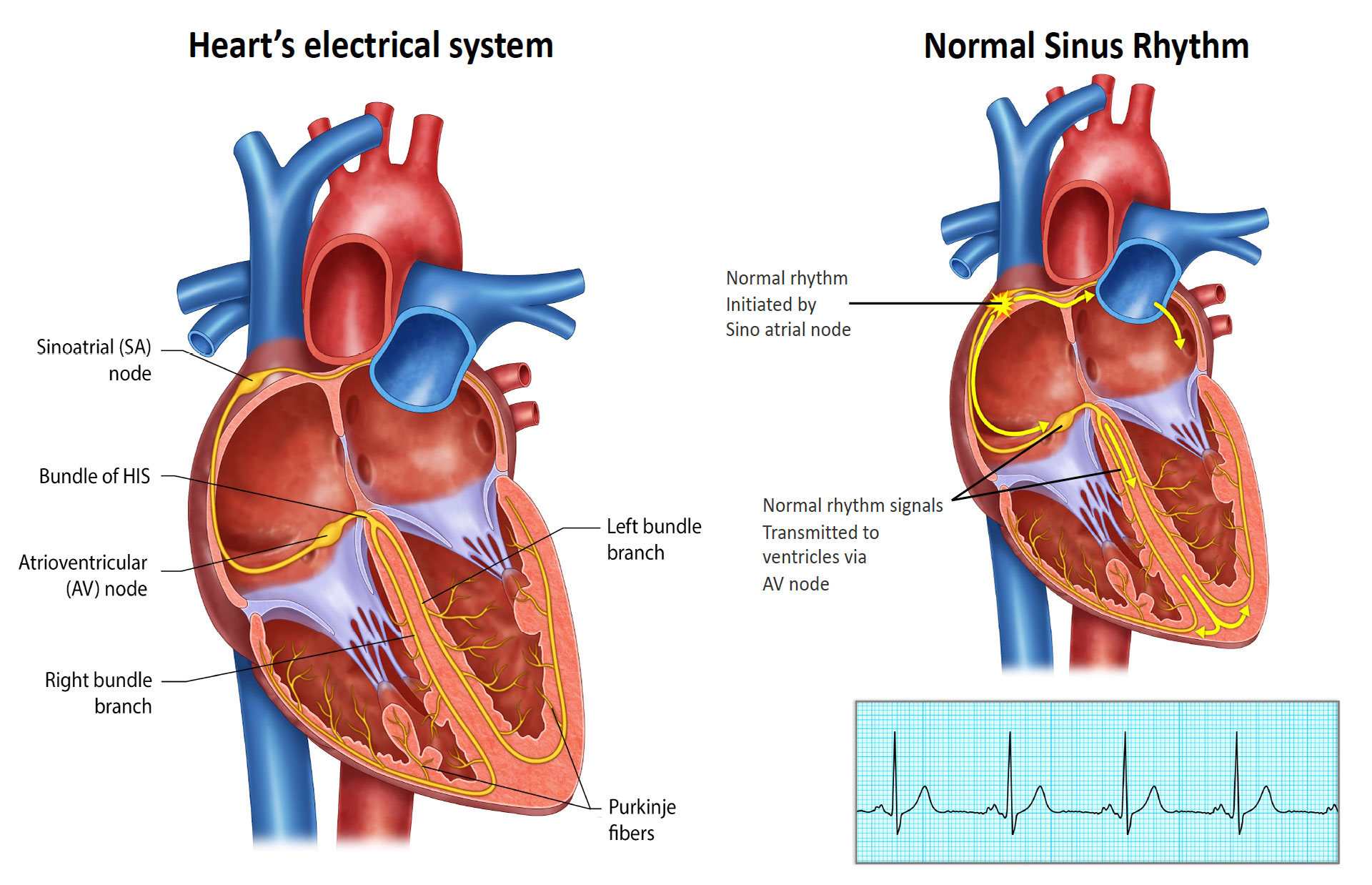
Atrial fibrillation is often referred to as AF or A-Fib. It is the most common abnormal rhythm worldwide. It is characterised by an irregular and often rapid heartbeat. It occurs when the upper chambers of the heart, known as the atria, experience chaotic electrical signals, causing them to quiver or fibrillate instead of contracting properly. As a result, the atria are unable to pump blood effectively into the lower chambers, called the ventricles. AF can result in stroke, heart failure, decreased quality of life, energy levels and exercise capacity.

How does AF start and manifest?
Atrial fibrillation (AF) can start and manifest in different ways. The exact triggers and underlying mechanisms may vary from person to person.
Initiation: AF can be triggered by abnormal electrical impulses originating in the atria (usually the pulmonary veins in the left atrium). These impulses disrupt the normal rhythm and coordination of the heart.
Manifestation: The symptoms of AF can vary among individuals. Some people may experience noticeable symptoms, while others may be asymptomatic and only discover their condition during routine medical check-ups. Common symptoms of AF include palpitations (sensations of irregular or rapid heartbeat), shortness of breath, decreased exercise tolerance, fatigue, dizziness or lightheadedness, chest discomfort or pain, and fainting. However, it’s important to note that some people with AF may have no apparent symptoms and the condition is detected through diagnostic tests.
It’s worth mentioning that AF can have significant health implications, including an increased risk of blood clots, stroke, and other complications. Therefore, it is important for individuals experiencing symptoms suggestive of AF or at risk of the condition to seek medical evaluation and guidance for proper diagnosis, management, and treatment.
What are the risk factors for atrial fibrillation?
Several risk factors can contribute to the development of atrial fibrillation. Here are some common risk factors:
Age: The risk of atrial fibrillation increases with age, particularly beyond the age of 60.
High blood pressure: Hypertension is a significant risk factor for AF. High blood pressure can damage the heart’s electrical system and increase the risk of abnormal heart rhythms.
Heart diseases: Various heart conditions, such as coronary artery disease, heart valve disorders, heart failure, and congenital heart defects, can increase the risk of atrial fibrillation.
Obesity: Excessive weight and obesity are associated with an increased likelihood of developing atrial fibrillation. Obesity can lead to other risk factors like high blood pressure and diabetes, which also contribute to AF.
Thyroid problems: Hyperthyroidism (overactive thyroid) or hypothyroidism (underactive thyroid) can increase the risk of atrial fibrillation.
Sleep apnoea: Sleep apnoea, a disorder characterized by interrupted breathing during sleep, has been linked to an increased risk of AF. The intermittent drops in blood oxygen levels, build-up of carbon dioxide and the resulting stress on the heart can contribute to the development of AF.
Alcohol consumption: Excessive alcohol intake, particularly binge drinking, is a known risk factor for atrial fibrillation. Alcohol can directly affect the heart’s electrical signalling and increase blood pressure.
Family history: A family history of atrial fibrillation increases the likelihood of developing the condition. Genetic factors may play a role in predisposing individuals to AF.
Other factors: Smoking, chronic lung diseases and previous heart surgeries can increase the risk of atrial fibrillation.
It’s important to note that having one or more of these risk factors does not necessarily mean a person will develop atrial fibrillation. However, individuals with multiple risk factors should be mindful and may benefit from lifestyle modifications and regular check-ups with their healthcare provider.
Why is AF a problem? What are potential consequences of AF?
Here are the main reasons why AF is a concern:
Irregular rapid heart rhythm: AF causes the atria (upper chambers of the heart) to quiver or fibrillate instead of contracting effectively. This irregular rhythm can result in a fast and chaotic heartbeat, which can be uncomfortable and unsettling. People can feel unwell when they go into AF with varying degrees of symptoms.
Blood clot formation & stroke: When the atria do not contract properly, blood can pool / stagnate in the chambers, increasing the risk of blood clots. These clots can break loose and travel through the bloodstream to various organs, particularly the brain, leading to a stroke. AF increases the risk of stroke by five times compared to individuals without AF. Strokes caused by AF tend to be more severe and have a higher risk of disability or death compared to other types of strokes.
Heart failure: The irregular and rapid heartbeat in AF can overwork the heart, leading to a weakened heart muscle over time. This can result in heart failure, where the heart cannot effectively pump blood to meet the body’s demands. Heart failure causes symptoms such as fatigue, shortness of breath, and fluid retention. In many cases, AF related heart failure and return to normal function with restoration and maintenance of sinus rhythm.
Reduced blood flow: The irregular and disorganized atrial contractions in AF can lead to inefficient blood flow. This can result in various symptoms such as shortness of breath. This can exacerbate or contribute to a condition called heart failure with preserved ejection fraction.
Impaired quality of life: AF can significantly impact a person’s quality of life. The symptoms of AF, such as palpitations, dizziness, fatigue, and shortness of breath, can limit physical activity, affect sleep, and cause anxiety or emotional distress.
Increased healthcare utilization: AF often requires medical intervention, monitoring, and management. This can result in frequent healthcare visits, diagnostic tests, and medications, which can place a burden on the healthcare system and increase healthcare costs.
It’s important to note that not everyone with AF will experience all of these consequences, and the severity can vary among individuals. However, the potential risks associated with AF emphasize the need for proper diagnosis, management, and treatment to reduce complications, improve quality of life, and prevent serious events like strokes.
Are there different types / patterns of AF?
The pattern of atrial fibrillation (AF) can vary, ranging from intermittent to continuous. Different terms, such as paroxysmal AF, persistent AF, and long-standing persistent AF, are used to describe these various patterns. Paroxysmal AF refers to episodes that occur intermittently, while persistent AF involves continuous episodes lasting more than 7 days.
AF is known to be a progressive condition, and individuals may transition from paroxysmal AF to persistent AF, and eventually to chronic AF, over time. The rate of progression is influenced by individual risk factors and can differ among people.
What is the long-term prognosis with AF?
The long-term prognosis of atrial fibrillation (AF) can vary depending on several factors, including the individual’s overall health, the presence of underlying heart conditions, and the effectiveness of treatment and management strategies.
It’s important to note that while AF can have significant implications, appropriate management and treatment can help improve outcomes and minimize the associated risks. Regular medical follow-ups, adherence to prescribed medications, lifestyle changes (such as maintaining a healthy weight, exercising regularly, and managing other health conditions), and compliance with treatment recommendations are crucial for optimizing the long-term prognosis for individuals with AF.
In many cases, once the correct management strategies and treatment have been instituted, you are expected to lead a normal life.
What are the treatment options available for AF?
Medications:
Medications are generally the first line treatment in the management of AF. Medications can be used for two reasons. First is to prevent a stroke. Second is to control your heart rhythm.
Medications used to prevent strokes are collectively referred to as anticoagulants. The necessity and duration of anticoagulant therapy vary and depend on factors such as age and other individual risk factors. The risk of stroke is often assessed using a commonly used scoring system called the CHA₂DS₂-VASc score.
Medications are also employed to control abnormal heart rhythms, either by stopping rapid heartbeats or regulating the heart rate. However, for individuals who experience ongoing episodes of AF despite medication use, have intolerances to prescribed medications, or prefer not to rely on long-term medication, procedural options may be considered. In certain cases, the use of medications may necessitate the placement of a pacemaker for safe administration.
There are multiple medications and combinations available that can be prescribed to address AF. Finding the most effective medication often involves a process of trial and adjustment of dosage and medication type to determine their efficacy. Regular monitoring is typically required for medications that target abnormal heart rhythms.
Heart rhythm medications can be used either on a regular basis or as needed in a “pill-in-pocket” strategy for acute AF episodes.
It is important to consult with your healthcare provider to determine the appropriate medication regimen for your specific situation. They will also provide guidance on dosage, medication adjustments, and the need for regular monitoring to ensure optimal management of AF.
What is pill-in-pocket approach?
The “pill-in-the-pocket” approach involves the as-needed use of prescribed antiarrhythmic medications, typically flecainide or sotalol. This strategy is utilized by individuals who experience relatively infrequent episodes of atrial fibrillation (AF). The goal is to terminate AF episodes without the need to go to the emergency department or hospital.
In this approach, the medication is taken if there is a suspicion that an AF episode has lasted more than 15 minutes. It’s important to note that these medications may take several hours to take effect. If you feel very unwell or if the episode persists for more than 24 hours, it is advisable to seek medical attention. It is crucial not to drive under these circumstances.
Please consult with your healthcare provider for personalised advice regarding the “pill-in-the-pocket” approach and to determine if it is appropriate and safe for your specific situation.
Procedural options:
An electrical cardioversion: In this procedure, an electrical shock is delivered to the heart through electrodes placed on the chest. The shock is synchronised with the heart’s electrical activity to ensure it is delivered during a specific phase of the cardiac cycle. The electrical energy briefly interrupts the abnormal heart rhythm and allows the heart’s natural pacemaker to re-establish a normal sinus rhythm. Electrical cardioversion is usually performed under sedation or general anaesthesia to minimize discomfort.
A Catheter ablation is commonly performed for AF.
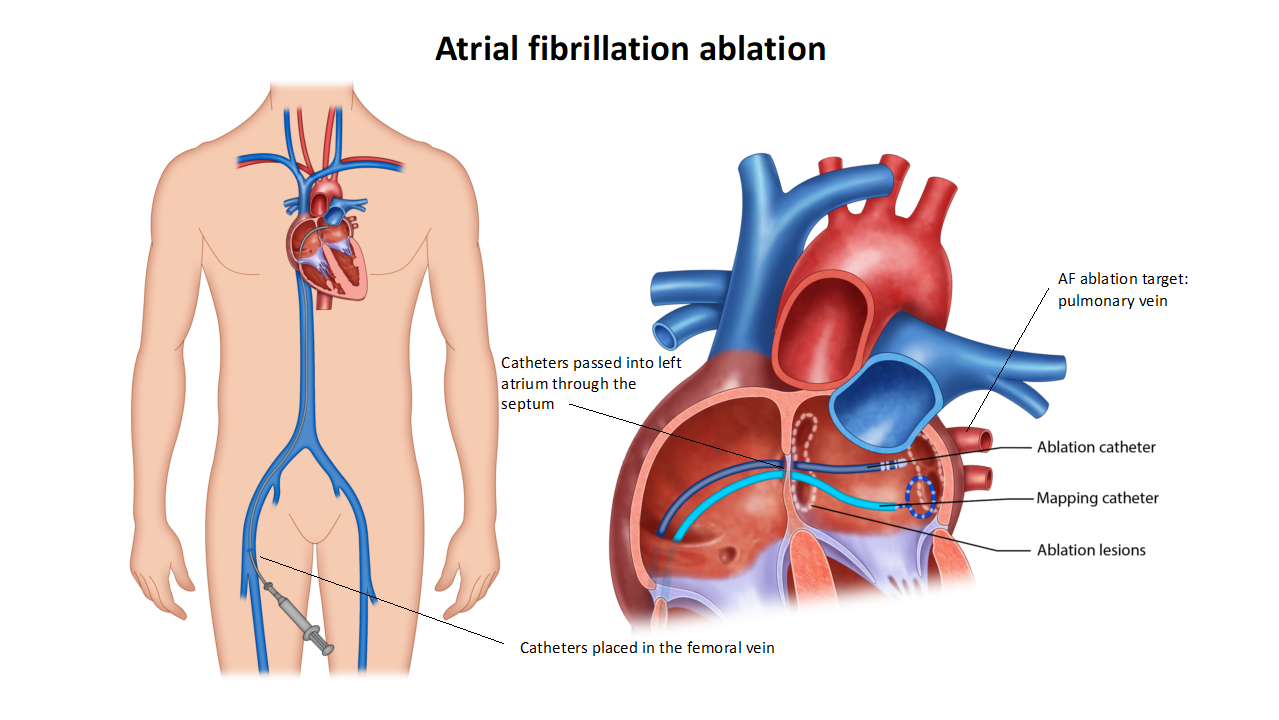
Refer to the AF ablation procedure section for more information.
Pacemaker and AV node ablation: The choice of a pacemaker implantation and atrioventricular (AV) node ablation is considered as a final treatment option when medications and other ablation procedures prove ineffective in controlling rapid heart rhythms associated with atrial fibrillation (AF). This treatment approach involves two steps.
First, a pacemaker is implanted to assist in regulating the heart’s rhythm. The pacemaker monitors the heart’s electrical activity and delivers electrical impulses as needed to maintain a stable and regular heartbeat.
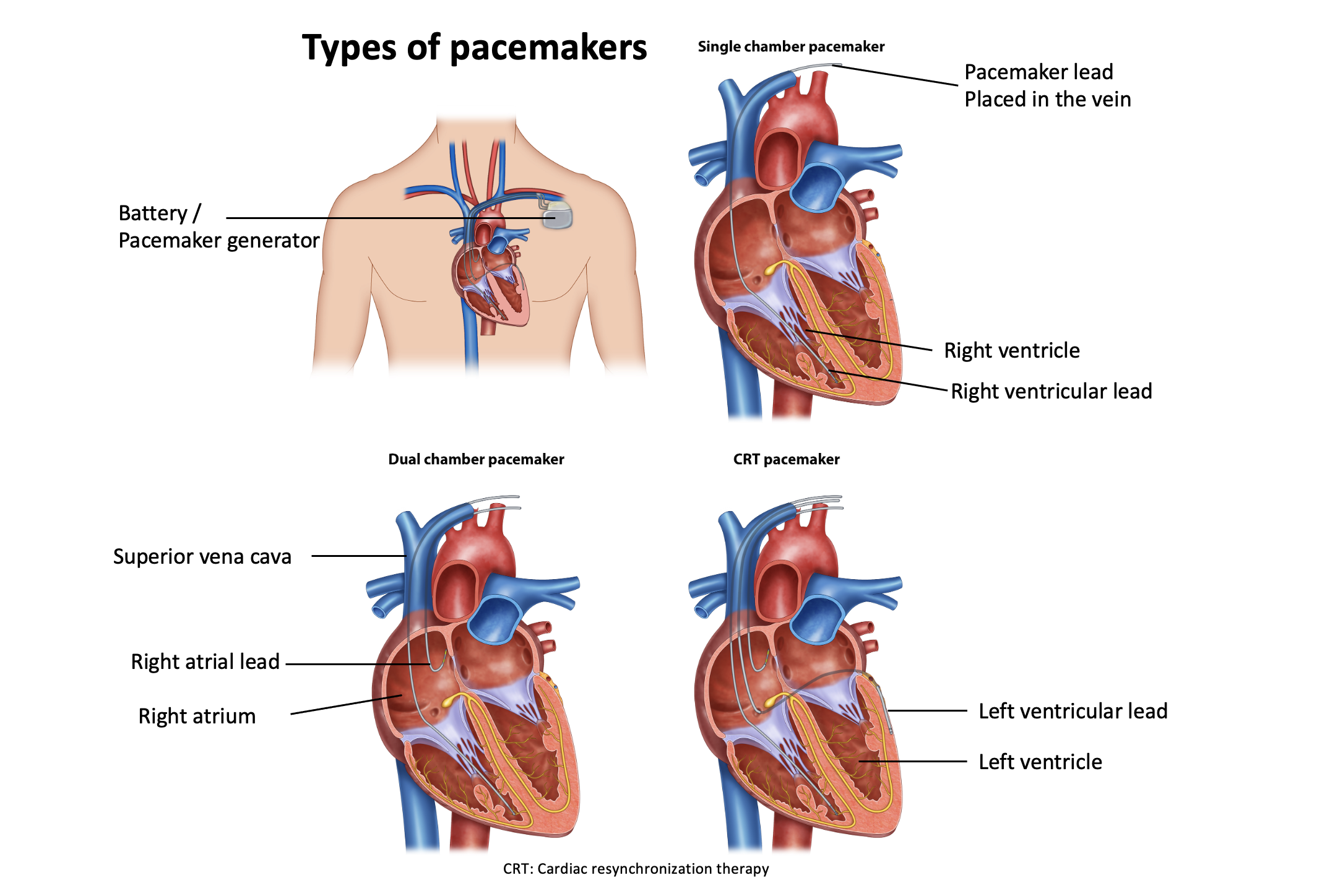
Following the pacemaker implantation, an AV node ablation procedure is performed several weeks later. During this procedure, the AV node, which is responsible for conducting electrical signals between the atria and ventricles, is intentionally ablated. This prevents the heart from beating in a disorganized manner caused by AF. The pacemaker then takes over the role of regulating the heart’s rhythm.
While AF continues to exist in the background, it no longer causes the heart to race. Long-term anticoagulant medication therapy is still necessary to prevent the risk of stroke associated with AF.
The decision to pursue pacemaker implantation and AV node ablation as a treatment option is made by a healthcare professional based on an individual’s specific circumstances and the severity of their AF-related rapid heart rhythms. Close monitoring and regular follow-up with the healthcare team are important after the procedure to ensure proper functioning of the pacemaker and ongoing management of AF.