Coronary Angiogram and PCI
What is a coronary angiogram?
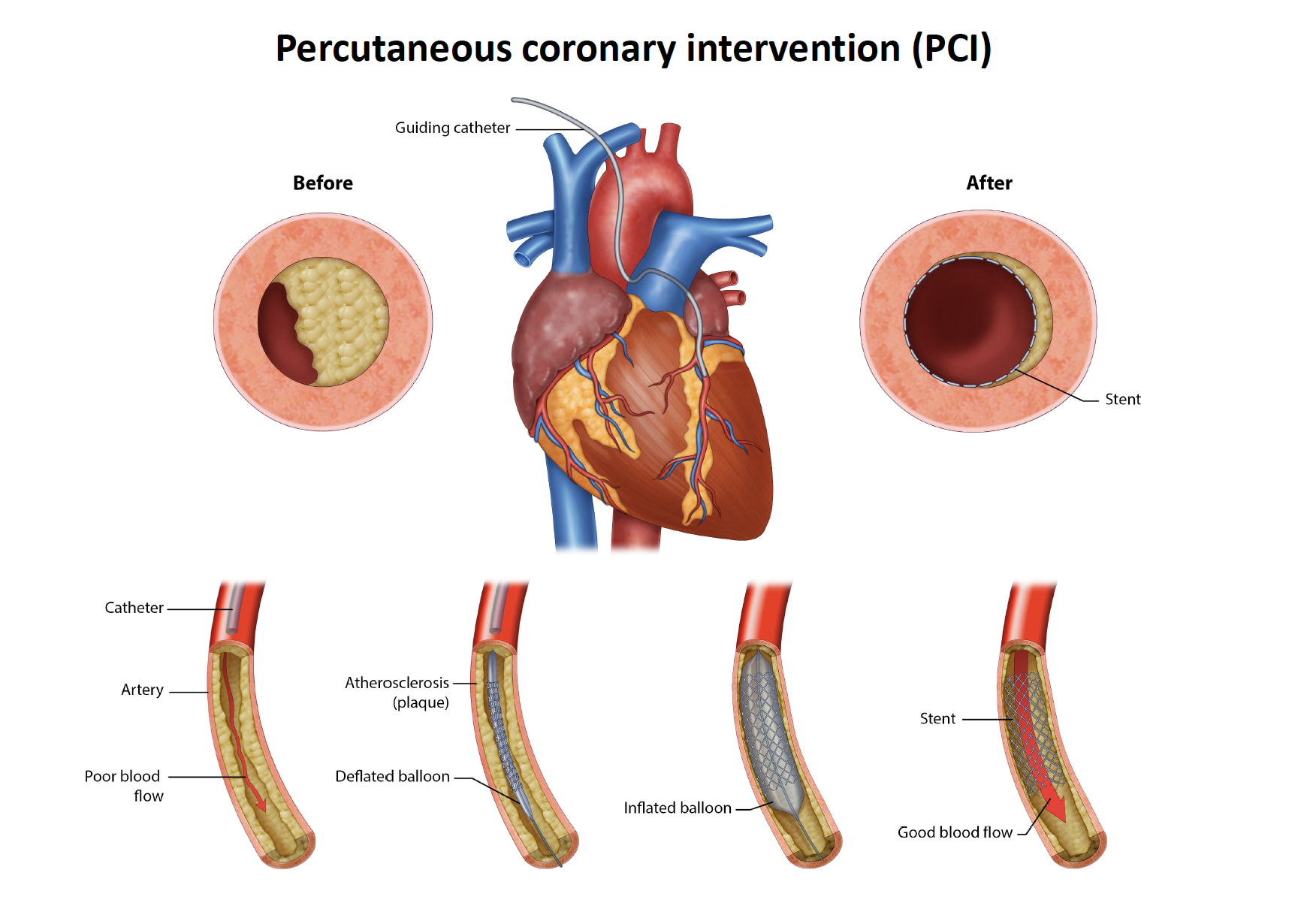
A coronary angiogram is a common procedure used to check the arteries (blood vessels) supplying your heart using X-ray and a special dye called contrast. The test is usually recommended to see if there’s a narrowing affecting the blood flow to the heart. Narrowing in the heart vessels can lead to angina which is chest/jaw/arm heaviness with exertion and if a heart vessel blocks acutely it can lead to a heart attack which can damage heart muscle if not treated urgently. Damage to heart muscle can have long term implications for patients so it is important to prevent them from occurring.
A coronary angiogram can be used both to diagnose and to treat blocked blood arteries. The procedure to fix/unblock the artery is called coronary angioplasty/stenting (PCI) which can be performed immediately following the diagnostic angiogram. On occasion the doctor will choose to stop after the angiogram and discuss the results with the patient and potentially a heart surgeon to determine what is the best treatment for that particular patient. That choice will be between open heart surgery (coronary bypass surgery) or the less invasive coronary stenting and in some cases, medications only will be recommended.
Coronary angiogram involves first placing a sheath into the artery (blood vessel) in your wrist or groin. Through the sheath a long thin tube will be placed and under X-ray guided into the arteries of your heart. A dye is injected and x-rays are taken. After the sheath is placed into the wrist or groin you should feel no pain during the procedure.

Why do I need a coronary angiogram?
Your doctor may recommend that you have a coronary angiogram if you have:
⦁ Myocardial infarction or heart attack – NSTEMI or STEMI
⦁ Symptoms of coronary artery disease, such as chest pain (angina), jaw, neck or arm that can’t be explained by other tests and may put you at increased risk of having a heart attack or is impacting on your ability to exercise.
⦁ A heart defect you were born with (congenital heart disease)
⦁ Abnormal non-invasive heart stress test
⦁ Prior to your planned cardiac surgery to determine the status of your coronary arteries
Due to the small risk of complications, angiograms aren’t usually done unless other non-invasive heart tests have been performed prior such as a stress test often involving echocardiogram or a CAT scan of your heart arteries which has diagnosed narrowings in the heart arteries.
What are the risks of a coronary angiogram?
Major complications are rare and about 1 in 1000.
Potential risks and complications include:
⦁ Myocardial infarction / heart attack
⦁ Stroke
⦁ Irregular heart rhythms (arrhythmias)
⦁ Allergic reactions to the dye
⦁ Allergy to medications used at the time of procedure
⦁ Kidney damage
⦁ Excessive bleeding from the groin or wrist
⦁ Infection
What is involved in having an Angiogram?
Your admission : On admission to the Cardiac Short Stay Unit, you will be greeted by members of a specialist cardiac healthcare team who will be caring for you before and after your procedure. It is expected that you will stay in hospital for the day or overnight, or until you have met the expected outcomes for your procedure. In preparation for your discharge, we will discuss what supports and potential needs you may have at home.
Your preparation:Please bring any medications you take (in their original packets) and show them to your admitting nurse. You will be given some paperwork to complete before admission if required. This information will help us to provide the right care for your specific needs. You may receive a call from the pre- admission clinic if we need to clarify any other details.
You will be given an information pack prior to procedure (or on arrival) depending on the time of the procedure and when you see the doctor. You must fast from food for six hours prior to your procedure.
You can have clear fluids up to two hours before your procedure. On the morning of your procedure, you should take any medications with a sip of water, unless you have been instructed to do otherwise.
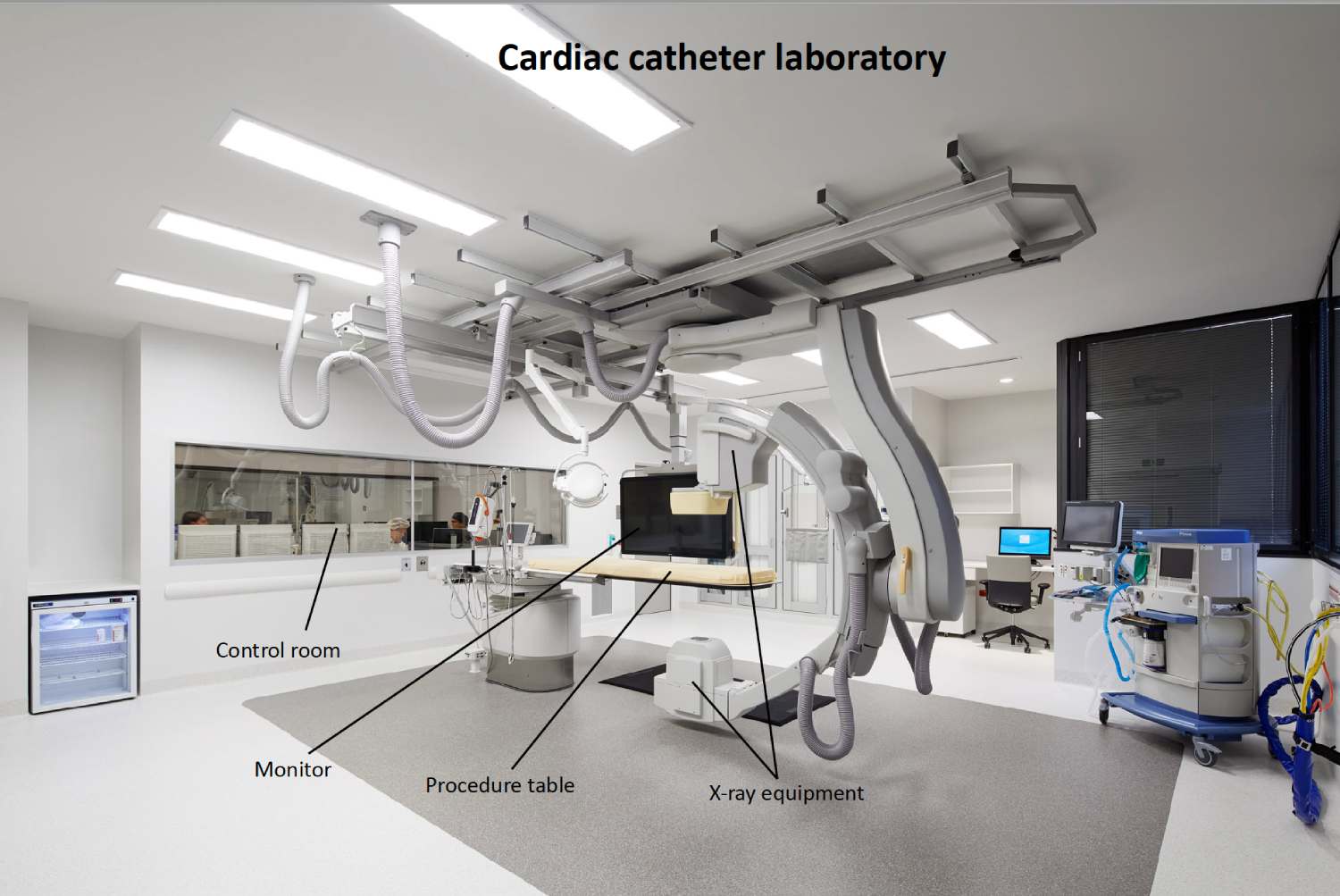
You will be asked to change into a hospital gown – underwear and jewellery should be removed. You may continue to wear your spectacles and dentures and tape over your wedding ring. Nail polish should also he removed. You will then be transferred to the Cardiac Catheter Laboratory with your nurse for your procedure.
During the procedure: You will be transferred to the Cardiac Catheter Laboratory (commonly called the Cath Lab) and positioned onto an X-ray table, which is quite narrow and firm. The procedure site will be shaved, usually right wrist and in some cases – both depending on the specialist.
The angiogram procedure usually takes about 30-60 minutes to complete. The angioplasty (PCI) usually takes 45-60 minutes. The catheters and sheath are then removed.
On completion of the procedure when access was obtained via the wrist you will likely have a plastic strap around your wrist (TR Band), which also contains air (15mls) this air is gradually removed over a period of a few hours.
When the groin was used as the access site the sheath will be removed and firm pressure will be applied to the skin, or, alternatively, a special plug/stitch (e.g. Angioseal, Proglide) will be inserted as the sheath is removed. You may also have a special ‘clamp’ on your groin (femstop), which contains air under pressure. This air is gradually removed over a period of 1-2 hours and then removed. After this you will often have to lie flat for 4-6 hours to reduce the risk of groin bruising
After the procedure: Your nurse will collect you from the catheter laboratory and return you to the Cardiac Short Stay Unit. You may feel drowsy for a few hours afterwards because of the sedation.
You may be connected to a heart monitor after your procedure. Your nurse will be checking your Blood pressure, pulse, operative site, foot pulses and circulation frequently after returning to the ward.
If there is a TR band around the wrist, then the nurse will be gradually removing air using a special syringe until the band is empty. The band may then be removed. If there is any further sign of bleeding, then this may be replaced for a period. Once the band is removed, the site is cleaned, and a small sterile dressing applied. Your nurse will ask you to report any chest or back discomfort as well as any swelling or discomfort from the puncture site.
During the period of observation, you should minimise movement of the arm or leg used in the procedure. Keep the leg that was used straight or have the arm that was used resting on a pillow and remain flat in bed as instructed by the nurse or Cardiologist. This is to allow the puncture site time to heal and to help prevent bleeding. You may bend your other leg and use your other arm. After about 2 hours, your nurse may allow you to sit up a little – DO NOT sit up until your nurse gives you the instruction. You will be allowed to eat and drink after the procedure but be aware when ordering that you will be lying flat. You will be offered sandwiches and other ‘finger food’ items after your return to the ward. Your nurse will assist you with any hygiene and toileting needs whilst you are in bed. Once you can get up, it is important that for the first time, you do so with your nurse, so that the puncture site can be monitored during and afterwards.
Discharge home: After 4-6 hours (once your nurse and/ or cardiologist is happy with your recovery), you should be able to get up and move around gently.
NOTE: If your cardiologist is happy with your progress, you will be discharged home on the day of your procedure.
Discharge time is early on morning after your procedure and following your doctor’s review. You should expect to be leaving the hospital by 08:30am. Please ensure your relative/friend is prepared to collect you and escort you home at this time.
Your nurse will present you with a discharge package containing information tailored to your needs, including care of the groin incision wound, about resuming normal activities, a list of any medications you may be on, and information on any new medications you may be starting.
Your regular medications will be returned to you on discharge, and you should receive an initial supply of any new medications.
You may be given the drug Glyceryl Trinitrate to take home with you. This comes as tablets – Anginine, or a spray – Nitrolingual. If you are given these it is important that you always carry a supply of fresh tablets or a spray with you (mark on the container the date you open a bottle of anginine, as those tablets remain effective for 90 days/3 months).
If you had a coronary stent inserted, you are normally prescribed an extra medication called Clopidogrel (commonly known as Plavix or Iscover) or Ticagrelor (commonly known as Brilinta) – these are anti-clotting medications which help your stent settle in position by modifying the body’s natural reaction to a foreign object (the metal stent) and reduce the risk of acute blockage of the stent. It is very important you stay on these medications and only stop them after discussion with your cardiologist.
If you had a coronary angioplasty, you will probably be referred for Cardiac Rehabilitation at a facility close to your home. You would normally be expected to see your cardiologist in 4-6 weeks. Before you are discharged an appointment may be made for you, or you may be given a card and asked to phone to make an appointment at a convenient time for you.
Recovery: information for you and your family
With a groin puncture you should only walk a little and plan to rest at home the following day. With a wrist puncture, you should use your arm sparingly for the next one-two days and avoid flexing the wrist for a minimum of 24 hours. Do not lift heavy weights for at least a week following the procedure. Your doctor will advise you about when you can drive.
You should be able to have a shower. When bathing or showering, do not rub soap or talcum powder over the puncture site. Allow water to run over it and pat dry. The plastic dressing over the puncture can normally be removed in the shower the day after the procedure. You should be able to eat normally.
Depending upon the results of the angiogram, or PCI, you may be commenced on a cardiac diet – essentially a low fat, low cholesterol, and low salt diet. You should drink plenty of fluids over the next eight hours as this helps to flush out the contrast used during the procedure. You should be passing urine normally and your usual bowel patterns will have returned. Observe the groin puncture site and note if there is any further swelling, bruising, redness, or discharge. Minor bruising may occur around the puncture site and can last 2 weeks. Do not worry about this. But if pain occurs over the puncture site or it becomes tender to touch, contact your doctor sooner.
Information to manage any bleeding:
- Lie down
- Apply continuous firm pressure with a clenched fist over the groin puncture site, or two fingers over a wrist puncture
- Maintain this pressure for 10-15 minutes or until bleeding stops
- Notify your doctor
If you develop further chest pain/ angina, take anginine spray/tablets as per the instructions below:
⦁ Always carry your fresh Anginine tablets or Nitrolingual spray with you
⦁ If angina occurs stop what you are doing. Stay calm!
⦁ Sit or lie down and rest for 2-3 minutes
⦁ If the pain is still there, take one dose of tablet or spray under the tongue. Remember DO NOT Swallow the tablet
⦁ Wait 2 minutes (it is important to wait to allow the medication to go into the bloodstream)
⦁ If you still have any discomfort after 5 minutes, take a second dose ⦁ Wait 5 minutes
⦁ If you still have any discomfort after 5 minutes, take a third dose IF you do not feel dizzy
⦁ IF THE DISCOMFORT CONTINUES CALL AN AMBULANCE PHONE 000
⦁ Wait for the ambulance. Do not allow family or friends to drive you to hospital
⦁ If the discomfort has been relieved by the medication rest awhile before resuming activity. Report to your doctor if this episode is more severe, or if the attacks are becoming more frequent.



